Can Medical Marijuana Help Patients Recover from Pneumonia?
What You Need to Know: Medical Cannabis for Pneumonia

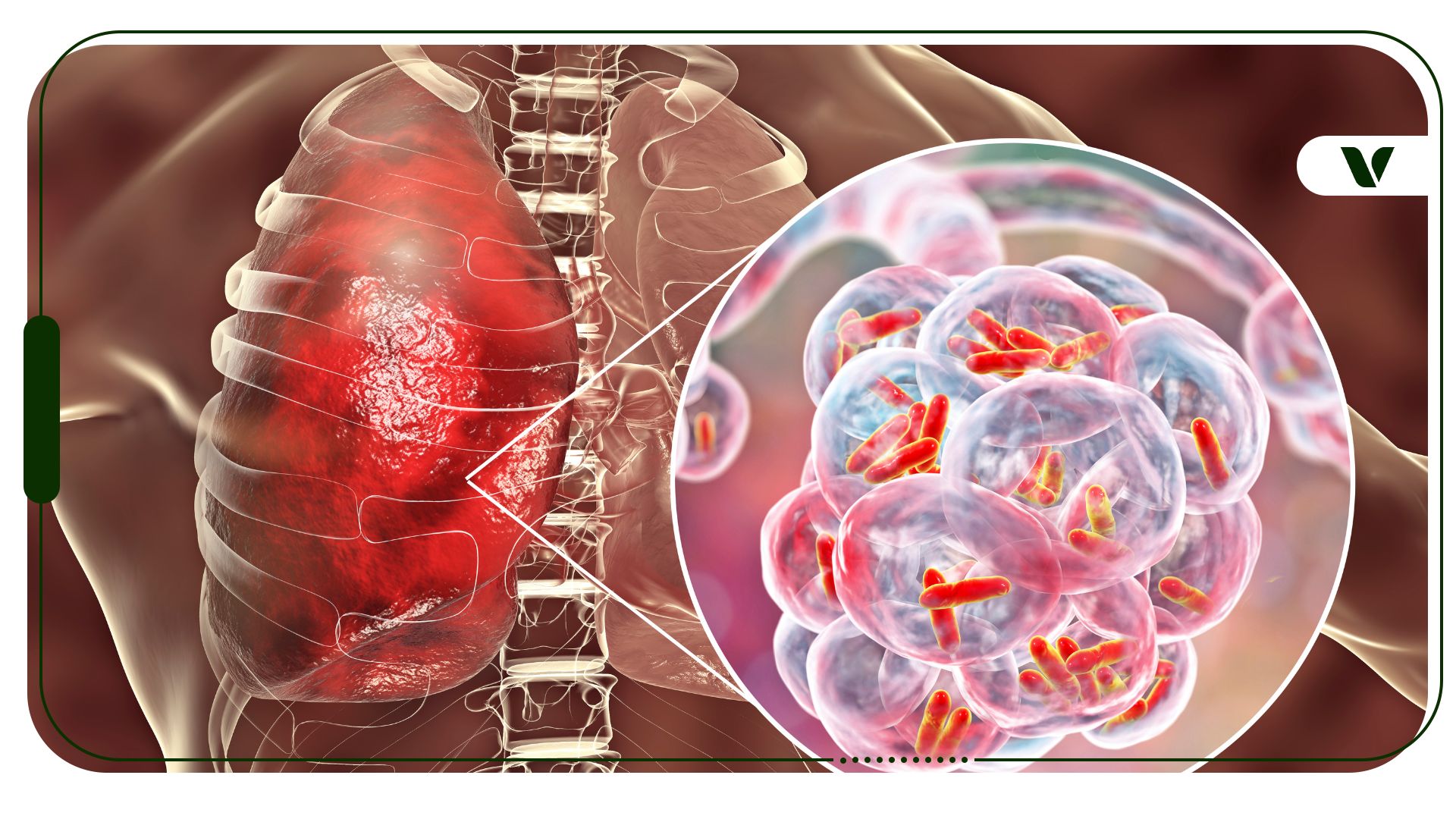
Photo Credit: iStock
The relationship between cannabis use and pneumonia is complex, as several factors—such as the type of pneumonia, smoking history, and immunity—influence it. Research has identified long-term marijuana smoking as a potential cause of pneumonia, though it does not appear to increase the risk of chronic obstructive pulmonary disease (COPD) or lung cancer.
Smoking cannabis daily or frequently, particularly due to the presence of Δ9-tetrahydrocannabinol (THC), affects immune cells in the alveoli and alters bronchial tissues, which leads to increased phlegm, coughing, and thus risk of microbial infection. Experts advise caution and recommend using alternative cannabis delivery methods, such as tinctures or edibles, to reduce lung irritation during pneumonia.
The activation of the endocannabinoid system (ECS) by cannabis, including THC and cannabidiol (CBD), can temporarily weaken immune responses and provide temporary bronchodilation. However, chronic cannabis use may constrict lung capacity over time. Experts discourage using cannabis during pneumonia, especially through smoking, because it can irritate the lungs and increase the risk of infection. This article emphasizes the need for further research to understand the nuanced effects of cannabis on pneumonia and highlights the importance of considering individual health conditions and methods of cannabis consumption.
The Science Behind Medical Cannabis for Pneumonia
- Cannabis Use and Pneumonia
- Can Cannabis Help Alleviate Symptoms of Pneumonia?
- How to Use Marijuana for Your Pneumonia Symptoms?
- Understanding the Different Types of Pneumonia
- Research on Pneumonia and Cannabis Use
Can Cannabis Help Alleviate Symptoms of Pneumonia?
Treating pneumonia with medical marijuana is complicated. Not only can the effects of it vary depending on the type of pneumonia you have, but it is also known to cause pneumonia in people who are daily or long-term marijuana smokers. Cannabis smoke does not appear to increase the risk of developing chronic obstructive pulmonary disease (COPD) or lung cancer. However, it is associated with symptoms of chronic bronchitis.
According to a 2015 expert panel review of the literature, “It is unclear whether cannabis is associated with an increased risk of pneumonia. Some case series and studies in immunocompromised patients have noted a link, but no definitive studies have been done. Some effects of smoked cannabis could predispose to pneumonia.”
The use of Δ9-tetrahydrocannabinol (THC) suppresses macrophages, a type of immune cell, and their functionality in alveoli, which are little air sacs that connect to the bronchioles and bronchi (where air enters the lungs). Alveoli are important because it’s the portion of the lung where your blood cells exchange carbon dioxide for fresh oxygen. THC also causes the ciliated, or hair-like, bronchial tissues to be replaced by hyperplastic mucus-secreting bronchial cells. This is related to the increased phlegm, smoker’s cough, and potential nidus of infection.
Cannabis begins its influence on the body through the activation of the endocannabinoid system (ECS), which is made up of fat-based neurotransmitters that the body self-produces. Through the activation of cannabinoid receptors in the body, the cannabinoids found in cannabis, such as THC and cannabidiol (CBD), can increase or decrease neurotransmitters and receptor activity in the body, allowing for immune modulation, pain reduction, and other physiological effects.
A 2018 evidence brief from the Michael G. DeGroote Centre for Medicinal Cannabis Research on the lungs and cannabis notes that both THC and the endocannabinoid anandamide (AEA)bind to CB1 receptors in the lungs, causing the smooth bronchial muscles to relax. This can help open up the airways into the lungs, but if THC is ingested and the airways are already relaxed, patients may experience bronchospasms, which restrict the airways. It is thought that acute use helps relax the bronchial muscles, but long-term cannabis use may actually constrict the lungs’ ability to take in air and exacerbate current lung disease, according to 2025 research.
To learn more about how the endocannabinoid system works, visit our page on endocannabinoids.
How To Use Marijuana For Your Pneumonia Symptoms?
Using medical cannabis while you have pneumonia can have different effects depending on a variety of factors. If you are a long-term cigarette or cannabis smoker, despite the evidence above about how cannabis can help open airways, any smoking will most likely cause you to have a harder time breathing or recovering while you have pneumonia.
Marijuana smoking or cigarette smoking can cause you to experience the following: increased coughing, increased mucus production, possible allergy to any contaminants, and increased risk for infection (23).
It is important to note that research supports that these issues can improve after smoking has stopped, so these changes are not necessarily permanent unless you are suffering from chronic lung disease or other cardiopulmonary complications (8). If you have any breathing-related symptoms or continue to suffer from the above symptoms after quitting, and it has been several months, please reach out to your health care provider to determine why you are having continued symptoms and best course of action. Shortness of breath or other breathing issues.
Tinctures, edibles, and topicals vaping, and edibles bypass airway routes completely. Dry herb or low-temp vaping offers more efficient and less irritating methods of delivery, while avoiding potentially hazardous free radicals and carbon monoxide from combustion. However, in medical marijuana, cannabis and pneumonia, pneumonia recovery, cannabis alternatives, THC effects on lungs, CBD for inflammation, cannabis safety, pneumonia types, cannabis immune response, lung health medical marijuana, cannabis and pneumonia, pneumonia recovery, cannabis alternatives, THC effects on lungs, CBD for inflammation, cannabis safety, pneumonia types, cannabis immune response, lung healthgeneral, inhalational methods are best avoided in patients with pneumonia or lung issues (8).
In general, medical marijuana may have the following positive lung health effects:
- Temporarily increase bronchodilation (17)
- Reduce chronic pain
- Reduce inflammation (caution in immunocompromised people)
- Antimicrobial effects against bacteria, viruses, and fungi
- Temporarily increases lung capacity
- Antianxiety and stress-relieving
Treating pneumonia with medical cannabis is not recommended by smoking or inhaling it because it can irritate the lungs, throat, and airways, and increase your risk for developing pneumonia over time (17). Smoking cannabis, like tobacco smoke, increases your risk of damage to your lungs over time, through profibrotic effects. It can also increase your body’s risk of health problems and infections, such as pneumonia, through its ability to modulate your immune system.
Through modulating your immune system, cannabis helps decrease chronic pain and inflammation by slowing down immune cell responses in B/T lymphocytes and macrophages, as well as altering the presence of cytokines (17). This may be great for people who have chronic inflammatory conditions, such as autoimmune diseases and arthritis, to slow the body’s attack on healthy tissue, but it can increase your risk for infection. Immunocompromised individuals may be more susceptible to microbial infections, including opportunistic infections like Aspergillus and Pseudomonas.
It is important to note that contaminated cannabis may sometimes contain bacteria and fungi that may also increase your risk of infection when inhaling cannabis, particularly if you have another chronic condition that lowers your immune system’s ability to fight off infections or are taking immunomodifying medications (17).
It is also unlikely, but possible, to be allergic to any contaminants like Aspergillus and Penicillium mold present on contaminated cannabis (17)(8). This is also noteworthy for persons with predisposing asthma or cystic fibrosis. All the more reason for everyone to double-check the lab quality of your cannabis before purchasing or consuming it.
READ: Concussion
What Is Pneumonia and What Causes It?
There are four main types of pneumonia; they are grouped by what is causing the infection. Healthcare providers may also further divide pneumonia into two groups: community-acquired vs healthcare-associated pneumonia, depending on the probable source of infection (2).
This distinction helps providers determine appropriate management and treatment per guidelines from the Centers for Disease Control & Prevention (CDC) and other professional societies (4). There are also many subtypes of each of the four main kinds that include new diagnoses like pneumonia caused by COVID-19 infection.

Photo Credit: iStock
The four main types include:
Bacterial Pneumonia
Bacterial pneumonia can be caused by a variety of different types of bacteria. It usually happens when the body has been weakened by illness, poor nutrition, or an impaired immune system. It is typically caused by pneumococci bacteria that are also responsible for ear infections, sinus infections, sepsis, and meningitis (24). You may also have an increased risk of pneumonia if you abuse alcohol, smoke cigarettes, or cannabis (18). Certain medical conditions, immune-reducing medications, and even surgery can also increase the risk of bacterial or other pneumonia.
Viral Pneumonia
Viral types of pneumonia are caused by viruses as opposed to bacteria. Influenza causes about one-third of viral pneumonia infections (18). If you suspect you have viral pneumonia, it is important to rest and take care of yourself because it can develop into bacterial pneumonia.
Breathing, pain, or any issues that worsen or fail to improve should be medically evaluated to rule out other potentially serious conditions. This is especially important in a COVID-19 world, and also emphasizes the need for vaccinations.
There are now safe and effective vaccinations for COVID-19 readily available in the US that prevent COVID pneumonia, hospitalization, and severe disease (9). Additionally, there are existing vaccines recommended by the CDC to prevent bacterial pneumonia in children under 5, people with certain risk conditions, 2 and persons over 50.65 (5). Antibiotics are not recommended for viral pneumonia, only bacterial pneumonia. Speak to your provider if you have any health concerns or questions about vaccines.
Mycoplasma Pneumonia
Also known as “walking pneumonia,” Mycoplasma pneumoniae are bacteria that can cause damage to the lining of the respiratory system and are considered contagious if you are in close contact with someone who has it (25). Outbreaks of walking pneumonia are common in crowded places like schools, dormitories, military barracks, nursing homes, and hospitals.
There is no specific vaccine available for this, but the best way to prevent this kind of illness is simply handwashing and covering coughs, as recommended by the CDC.
Atypical Pneumonia
These types of pneumonia are harder to diagnose through standard bacterial identification methods. They also can cause slightly different symptoms, appear differently in chest x-rays, or respond to antibiotics differently than the more typical types of pneumonia (26). Some atypical types can be caused by the following bacteria:
- Chlamydia pneumoniae – This is a type of bacteria that causes respiratory infections in children, which usually leads to mild pneumonia or bronchitis (3). Some people may be infected with this bacterium and have mild or no symptoms. Sometimes it is also referred to as Chlamydophila pneumoniae.
- Chlamydia psittaci – Also known as psittacosis, this bacterium is known for infecting birds, but it can sometimes be passed to people (27). It is important to follow good precautions while cleaning and handling birdcages to help avoid this infection. It can cause a mild respiratory illness or pneumonia in people.
- Legionella pneumophila – Legionnaires’ disease is a very serious type of pneumonia to be infected with. It is caused by swallowing or inhaling small water droplets that contain Legionella (28). Legionella occurs naturally in lakes and streams, but it becomes a health concern when it grows and spreads in building water systems, air conditioners, and hot tubs that are not properly cleaned and maintained. According to the CDC, 1 out of 10 people with Legionnaires’ will die from it – but this risk increases to 1 out of 4 if acquired in a healthcare facility.
Research on Pneumonia and Cannabis Use
According to a report given at the 2020 CHEST Conference, COPD patients saw a 37.6% reduction in the odds of dying in the hospital in patients with cannabis use (29). In addition, the same COPD patients had an 11.8% lower risk of developing pneumonia.
Another recent study evaluated cannabis use with the risk of pneumonia in men with human immunodeficiency virus (HIV), which came with similar results as above. This study checked in with patients at regular six-month intervals over the course of 30 years. Self-reported cannabis smoking daily or weekly did not increase the risk for pneumonia in the control group that included participants without HIV. (30). Patients with HIV saw a small increase in the risk of PCP (Pneumocystis carinii) pneumonia, which researchers think is thought to have to do with this group’s compromised immune system combined with the immune-suppressing effects of THC.
Frequently Asked Questions
What Helps Heal Lungs After Pneumonia?
Rest, hydration, breathing exercises, and avoiding lung irritants like smoke help support healing. Some people require recovery with pulmonary rehabilitation, fluids, and antibiotics only if appropriate.
Can Pneumonia Be Treated With Drugs?
Yes, depending on the cause, bacterial pneumonia is typically treated with antibiotics (for bacterial infections) or antivirals (for certain viral types), along with supportive and rehabilitative care. Antipyretics like acetaminophen and ibuprofen may alleviate body aches and fever, while cough suppressants may relieve breathing symptoms and mechanical chest pain.
Can Medical Marijuana Help Coughing?
Some cannabis compounds, like CBD and CBG, may reduce inflammation, but smoking can worsen coughing. Safer alternatives to address coughing would be edibles, or tinctures, or topicals. However, any ongoing symptoms or self-administered drugs should be shared with your medical provider.
When Can I Smoke Again After Pneumonia?
It is best to avoid smoking entirely during and after recovery, as it can irritate healing lung tissue and delay full recovery. Vaping may be gentler on the airways, but non-inhalational routes are the best and edibles are a good alternative if you are looking to benefit from the anti-inflammatory and pain-relieving properties of cannabis compounds.
What Supplements Help Recovery From Pneumonia?
Vitamin C, vitamin D, zinc, and antioxidants have the potential to support immune function and act as potential preventive measures. But these should be discussed with your doctor and should be used in conjunction with medical advice, not as an alternative.
What is the Best Drug for Pneumonia?
The cause of pneumonia determines what treatment will be best for the condition. Certain antibiotics (like azithromycin or amoxicillin) are good for bacterial pneumonia, and viral pneumonia responds to antivirals for certain viral types.
Still, drugs for pneumonia aren’t always necessary in healthy persons who have adequate nutrition, hydration, and rest. Your doctor will decide what kind of pneumonia you have and what you should take for it, if anything.
What Food Should Be Avoided in Pneumonia?
Avoid processed foods, excess sugar, and dairy, as these may worsen mucus production and inflammation. Focus on nutrient-rich, anti-inflammatory foods instead. Stay Hhydrated, too, as dehydration and malnourishment can lead to serious complications.
Note: The content on this page is for informational purposes only and is not intended to be professional medical advice. Do not attempt to self-diagnose or prescribe treatment based on the information provided. Always consult a physician before making any decision on the treatment of a medical condition.
References
- Blaskovich, M. A., Kavanagh, A. M., Elliott, A. G., Zhang, B., Ramu, S., Amado, M., Lowe, G. J., Hinton, A. O., Pham, D. M., Zuegg, J., Beare, N., Quach, D., Sharp, M. D., Pogliano, J., Rogers, A. P., Lyras, D., Tan, L., West, N. P., Crawford, D. W., … Thurn, M. (2021). The antimicrobial potential of cannabidiol. Communications Biology, 4(1). https://www.nature.com/articles/s42003-020-01530-y
- Centers for Disease Control and Prevention. (2020, October 22). Causes of Pneumonia. Centers for Disease Control and Prevention. https://www.cdc.gov/pneumonia/causes.html
- Centers for Disease Control and Prevention. (2019, January 10). Chlamydia pneumoniae: Causes, How It Spreads, and Risk Factors. Centers for Disease Control and Prevention. https://www.cdc.gov/pneumonia/atypical/cpneumoniae/about/causes.html
- Centers for Disease Control and Prevention. (2018, October 22). Pneumonia management and prevention guidelines. Centers for Disease Control and Prevention. Retrieved October 10, 2021, from https://www.cdc.gov/pneumonia/management-prevention-guidelines.html
- Centers for Disease Control and Prevention. (2020, August 7). Pneumococcal vaccination: What everyone should know. Centers for Disease Control and Prevention. Retrieved October 10, 2021, from https://www.cdc.gov/vaccines/vpd/pneumo/public/index.html
- Colli, M. (n.d.). COVID-19 Lung Inflammation Reduced by CBD. Cannabis Science Tech.https://www.cannabissciencetech.com/view/covid-19-lung-inflammation-reduced-by-cbd
- Esteitie, R., Inaty, H., & Qawi, I. (2013). Desquamative Inflammatory Pneumonia Caused by Marijuana. Chest, 144(4).https://journal.chestnet.org/article/S0012-3692(16)43082-5/fulltext
- Fugh-Berman, A., MD, Wood, S., PhD, Kogan, M., MD, Abrams, D., MD, Mathre, M., RN, MSN, CARN, Robie, A., MEd, . . . D’Antonio,, P., RPh, MS, MBA. (n.d.). An Introduction to the Biochemistry & Pharmacology of Medical Cannabis. Retrieved July 13, 2021, from http://docplayer.net/36028206-Medical-cannabis-adverse-effects-drug-interactions.html
- Harvard Health Publishing. (2021, October 8). Covid-19 vaccines. Harvard Health. Retrieved October 10, 2021, from https://www.health.harvard.edu/covid-19/covid-19-vaccines
- Hernández-Cervantes, R., Méndez-Díaz, M., Prospéro-García, Ó., & Morales-Montor, J. (2018). Immunoregulatory Role of Cannabinoids during Infectious Disease. Neuroimmunomodulation, 24(4-5), 183–199. https://www.karger.com/Article/Fulltext/481824
- La Grassa, J. (2020, February 28). Ontario researchers find cannabis has antibiotic potential | CBC News. CBCnews.https://www.cbc.ca/news/canada/hamilton/mcmaster-cannabis-antibiotic-1.5476869
- Lutchmansingh, D., Pawar, L., & Savici, D. (2014). Legalizing Cannabis: A physician’s primer on the pulmonary effects of marijuana. Current respiratory care reports, 3(4), 200–205. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4226845/
- Martinasek, M. P., McGrogan, J. B., & Maysonet, A. (2016, November). A Systematic Review of the Respiratory Effects of Inhalational Marijuana. Respiratory Care. http://www.dfaf.org/wp-content/uploads/2018/09/Martinasek-et-al.-2016-Resp-Care.pdf
- Merrick C.M., LeBlanc J.J. (2020) Cannabis in Pulmonary Medicine. In: Finn K. (eds) Cannabis in Medicine. Springer, Cham.https://link.springer.com/chapter/10.1007%2F978-3-030-45968-0_8
- Moir, D., Rickert, W. S., Levasseur, G., Larose, Y., Maertens, R., White, P., & Desjardins, S. (2008). A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chemical research in toxicology, 21(2), 494–502. https://pubmed.ncbi.nlm.nih.gov/18062674/
- Norml. (2020, August 13). Study: Marijuana Use Not Associated with Increased Risk of Pneumonia. NORML.https://norml.org/news/2020/08/13/study-marijuana-use-not-associated-with-increased-risk-of-pneumonia/
- Parihar, V. (2018, April 27). What effects does smoking cannabis have on the respiratory system?https://cannabisresearch.mcmaster.ca/news/2018/04/27/cannabis-smoking-and-effects-on-the-respiratory-system
- Pneumonia. Johns Hopkins Medicine. (n.d.). https://www.hopkinsmedicine.org/health/conditions-and-diseases/pneumonia
- Price, S. (2020, October 21). CBD reduces COVID-19 lung damage with protective peptides. Health Europa.https://www.healtheuropa.eu/cbd-reduces-covid-19-lung-damage-with-protective-peptides/103374/
- Ribeiro, L., & Ind, P. W. (2018). Marijuana and the lung: hysteria or cause for concern? Breathe, 14(3), 196–205.https://breathe.ersjournals.com/content/14/3/196
- Roth, M. D. (2015, February 1). Marijuana smoke promotes dysfunctional macrophage responses to HIV and pneumonia. Grantome.https://grantome.com/grant/NIH/R01-DA037102-02
- Susman, E. (2020, October 21). Marijuana Use Linked to Lower Hospital Mortality in COPD Patients. Medical News.https://www.medpagetoday.com/meetingcoverage/chest/89242
- Yayan, J., & Rasche, K. (2016). Damaging Effects of Cannabis Use on the Lungs. Advances in experimental medicine and biology, 952, 31–34. https://pubmed.ncbi.nlm.nih.gov/27573646/
- Pneumococcal infections. (2021, March 25). Retrieved October 10, 2021, from https://medlineplus.gov/pneumococcalinfections.html
- Mycoplasma pneumoniae causes and transmission. (2020, June 05). Retrieved October 10, 2021, from https://www.cdc.gov/pneumonia/atypical/mycoplasma/about/causes-transmission.html
- Atypical pneumonia. (2019, October 01). Retrieved October 10, 2021, from https://www.cdc.gov/pneumonia/atypical/index.html
- Psittacosis. (2019, August 22). Retrieved October 10, 2021, from https://www.cdc.gov/pneumonia/atypical/psittacosis/index.html
- Legionnaires’ disease and Pontiac fever. (2021, March 25). Retrieved October 10, 2021, from https://www.cdc.gov/legionella/index.html
- Susman, E. (2020, October 21). Marijuana use is linked to lower hospital mortality in COPD patients. Retrieved October 10, 2021, from https://www.medpagetoday.com/meetingcoverage/chest/89242?vpass=1
- Quint, J. J., Tashkin, D. P., McKay, H. S., Plankey, M. W., Stosor, V., Friedman, M. R., & Detels, R. (2020). Marijuana use and pneumonia risk in a cohort of HIV-infected and HIV-uninfected men. Annals of epidemiology, 52, 64–70.e2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7725997/
1. Blaskovich, M. A., Kavanagh, A. M., Elliott, A. G., Zhang, B., Ramu, S., Amado, M., Lowe, G. J., Hinton, A. O., Pham, D. M., Zuegg, J., Beare, N., Quach, D., Sharp, M. D., Pogliano, J., Rogers, A. P., Lyras, D., Tan, L., West, N. P., Crawford, D. W., … Thurn, M. (2021). The antimicrobial potential of cannabidiol. Communications Biology, 4(1). https://www.nature.com/articles/s42003-020-01530-y
2. Centers for Disease Control and Prevention. (2020, October 22). Causes of Pneumonia. Centers for Disease Control and Prevention. https://www.cdc.gov/pneumonia/causes.html
3. Centers for Disease Control and Prevention. (2019, January 10). Chlamydia pneumoniae: Causes, How It Spreads, and Risk Factors. Centers for Disease Control and Prevention. https://www.cdc.gov/pneumonia/atypical/cpneumoniae/about/causes.html
4. Centers for Disease Control and Prevention. (2018, October 22). Pneumonia management and prevention guidelines. Centers for Disease Control and Prevention. Retrieved October 10, 2021, from https://www.cdc.gov/pneumonia/management-prevention-guidelines.html
5. Centers for Disease Control and Prevention. (2020, August 7). Pneumococcal vaccination: What everyone should know. Centers for Disease Control and Prevention. Retrieved October 10, 2021, from https://www.cdc.gov/vaccines/vpd/pneumo/public/index.html
6. Colli, M. (n.d.). COVID-19 Lung Inflammation Reduced by CBD. Cannabis Science Tech. https://www.cannabissciencetech.com/view/covid-19-lung-inflammation-reduced-by-cbd
7. Esteitie, R., Inaty, H., & Qawi, I. (2013). Desquamative Inflammatory Pneumonia Caused by Marijuana. Chest, 144(4). https://journal.chestnet.org/article/S0012-3692(16)43082-5/fulltext
8. Fugh-Berman, A., MD, Wood, S., PhD, Kogan, M., MD, Abrams, D., MD, Mathre, M., RN, MSN, CARN, Robie, A., MEd, . . . D’Antonio,, P., RPh, MS, MBA. (n.d.). An Introduction to the Biochemistry & Pharmacology of Medical Cannabis. Retrieved July 13, 2021, from http://docplayer.net/36028206-Medical-cannabis-adverse-effects-drug-interactions.html
9. Harvard Health Publishing. (2021, October 8). Covid-19 vaccines. Harvard Health. Retrieved October 10, 2021, from https://www.health.harvard.edu/covid-19/covid-19-vaccines
10. Hernández-Cervantes, R., Méndez-Díaz, M., Prospéro-García, Ó., & Morales-Montor, J. (2018). Immunoregulatory Role of Cannabinoids during Infectious Disease. Neuroimmunomodulation, 24(4-5), 183–199. https://www.karger.com/Article/Fulltext/481824
11. La Grassa, J. (2020, February 28). Ontario researchers find cannabis has antibiotic potential | CBC News. CBCnews. https://www.cbc.ca/news/canada/hamilton/mcmaster-cannabis-antibiotic-1.5476869
12. Lutchmansingh, D., Pawar, L., & Savici, D. (2014). Legalizing Cannabis: A physician’s primer on the pulmonary effects of marijuana. Current respiratory care reports, 3(4), 200–205. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4226845/
13. Martinasek, M. P., McGrogan, J. B., & Maysonet, A. (2016, November). A Systematic Review of the Respiratory Effects of Inhalational Marijuana. Respiratory Care. http://www.dfaf.org/wp-content/uploads/2018/09/Martinasek-et-al.-2016-Resp-Care.pdf
14. Merrick C.M., LeBlanc J.J. (2020) Cannabis in Pulmonary Medicine. In: Finn K. (eds) Cannabis in Medicine. Springer, Cham. https://link.springer.com/chapter/10.1007%2F978-3-030-45968-0_8
15. Moir, D., Rickert, W. S., Levasseur, G., Larose, Y., Maertens, R., White, P., & Desjardins, S. (2008). A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions. Chemical research in toxicology, 21(2), 494–502. https://pubmed.ncbi.nlm.nih.gov/18062674/
16. Norml. (2020, August 13). Study: Marijuana Use Not Associated with Increased Risk of Pneumonia. NORML. https://norml.org/news/2020/08/13/study-marijuana-use-not-associated-with-increased-risk-of-pneumonia/
17. Parihar, V. (2018, April 27). What effects does smoking cannabis have on the respiratory system? https://cannabisresearch.mcmaster.ca/news/2018/04/27/cannabis-smoking-and-effects-on-the-respiratory-system
18. Pneumonia. Johns Hopkins Medicine. (n.d.). https://www.hopkinsmedicine.org/health/conditions-and-diseases/pneumonia
19. Price, S. (2020, October 21). CBD reduces COVID-19 lung damage with protective peptides. Health Europa. https://www.healtheuropa.eu/cbd-reduces-covid-19-lung-damage-with-protective-peptides/103374/
20. Ribeiro, L., & Ind, P. W. (2018). Marijuana and the lung: hysteria or cause for concern? Breathe, 14(3), 196–205. https://breathe.ersjournals.com/content/14/3/196
21. Roth, M. D. (2015, February 1). Marijuana smoke promotes dysfunctional macrophage responses to HIV and pneumonia. Grantome. https://grantome.com/grant/NIH/R01-DA037102-02
22. Susman, E. (2020, October 21). Marijuana Use Linked to Lower Hospital Mortality in COPD Patients. Medical News. https://www.medpagetoday.com/meetingcoverage/chest/89242
23. Yayan, J., & Rasche, K. (2016). Damaging Effects of Cannabis Use on the Lungs. Advances in experimental medicine and biology, 952, 31–34. https://pubmed.ncbi.nlm.nih.gov/27573646/
24. Pneumococcal infections. (2021, March 25). Retrieved October 10, 2021, from https://medlineplus.gov/pneumococcalinfections.html
25. Mycoplasma pneumoniae causes and transmission. (2020, June 05). Retrieved October 10, 2021, from https://www.cdc.gov/pneumonia/atypical/mycoplasma/about/causes-transmission.html
26. Atypical pneumonia. (2019, October 01). Retrieved October 10, 2021, from https://www.cdc.gov/pneumonia/atypical/index.html
27. Psittacosis. (2019, August 22). Retrieved October 10, 2021, from https://www.cdc.gov/pneumonia/atypical/psittacosis/index.html
28. Legionnaires disease and Pontiac fever. (2021, March 25). Retrieved October 10, 2021, from https://www.cdc.gov/legionella/index.html
29. Susman, E. (2020, October 21). Marijuana use linked to lower hospital mortality in COPD patients. Retrieved October 10, 2021, from https://www.medpagetoday.com/meetingcoverage/chest/89242?vpass=1
30. Quint, J. J., Tashkin, D. P., McKay, H. S., Plankey, M. W., Stosor, V., Friedman, M. R., & Detels, R. (2020). Marijuana use and pneumonia risk in a cohort of HIV-infected and HIV-uninfected men. Annals of epidemiology, 52, 64–70.e2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7725997/