Stiff Person Syndrome (SPS) is a rare and complex neurological and autoimmune disorder. It causes increasing muscle rigidity and leads to episodes of intense, painful muscle spasms, significantly impacting those affected.
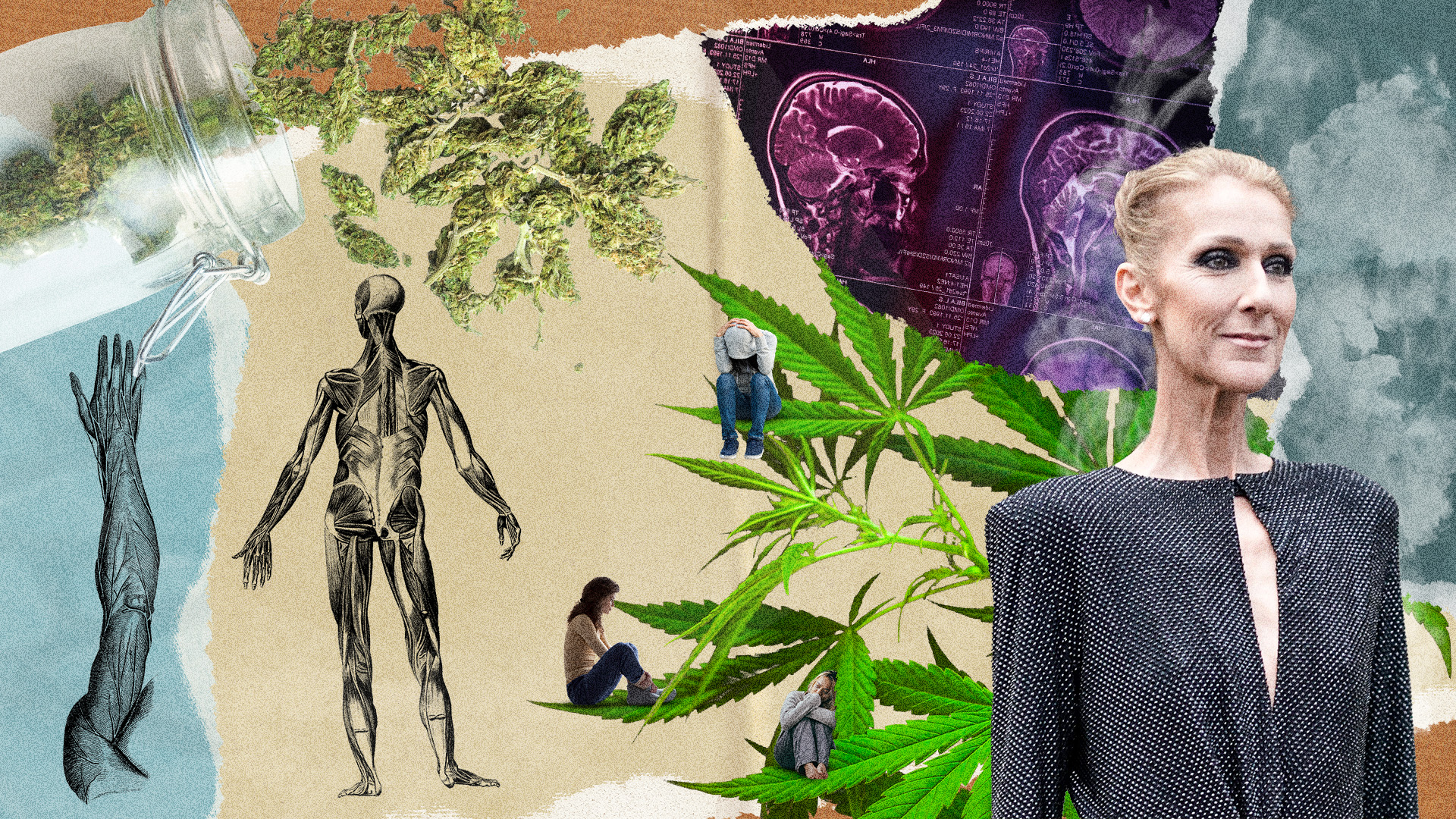
In December 2022, the well-known singer Celine Dion announced her struggle with SPS, drawing widespread attention to this condition. Naturally, this has sparked new conversations about treatments. One such promising area is the use of medical cannabis.
In this article, we delve into how cannabis could potentially ease the challenging symptoms of SPS, offering hope to many.
Understanding Stiff Person Syndrome
SPS is characterized by severe spasms of the face, torso, and limbs, accompanied by debilitating muscle stiffness. These symptoms fluctuate but significantly impact daily activities and mental health. As stated by Celine Dion, “The spasms affect every aspect of my daily life, sometimes causing difficulties when I walk and not allowing me to use my vocal cords to sing the way I’m used to,” she explained. “I have to admit it’s been a struggle. All I know is singing. It’s what I’ve done all my life.”
SPS often coexists with other serious illnesses, including cancers. However, a distinctive aspect of SPS is its immune-mediated nature. It’s mainly associated with antibodies to glutamic acid decarboxylase (GAD). GAD is a crucial nervous system enzyme that produces a neurotransmitter that helps regulate muscle tone. The disruption caused by these antibodies leads to the characteristic muscular rigidity and spasms of SPS.
GAD antibodies are detectable in SPS patients around 70-80% of the time. But it’s important to note that the absence of GAD antibodies doesn’t rule out the disease. When there are classic SPS symptoms but no detectable antibodies, it is called “seronegative” SPS.
Another type of SPS is called “paraneoplastic” SPS, which results from developing various types of cancer. It is estimated that up to 10% of SPS cases are associated with cancers like breast, colon, thyroid, lung, and Hodgkin and non-Hodgkin lymphomas.
There are a few other subtypes or partial variants of SPS including stiff limb, jerky SPS, cerebellar variant SPS with epilepsy, and dystonia.
Challenges in Treating SPS
Tackling SPS requires a multifaceted approach to treatment and is important for preventing permanent disability and mortality. Doctors commonly prescribe immunotherapy, which aims to regulate the immune system’s response and treat the underlying disease.
Additionally, medications that influence GABA, a key neurotransmitter in the brain, are used to manage muscular spasms and stiffness symptoms. While these treatments can alleviate some symptoms, their effectiveness varies significantly from one patient to another. Corticosteroids can also be hit or miss. Unfortunately, complete remissions of SPS are rare, making the journey towards effective management challenging.
Beyond the physical distress, SPS also exerts a profound psychological impact. Many patients live with anticipatory anxiety, constantly bracing for the next painful spasm. This anxiety can escalate into specific phobias, particularly in situations where symptoms might be triggered. For instance, a patient might develop a fear of being in crowded places, worried that the noise and activity could induce spasms. As a result, understanding and addressing both the physical and psychological aspects of SPS are crucial in providing comprehensive care to those affected.
Further complicating patients’ lives is that SPS is also usually associated with other autoimmune and hormonal (endocrine) disorders like diabetes, celiac, thyroid disease, vitiligo, and pernicious anemia. This makes treatment even more difficult and cumbersome for patients.
Why You Should Get Your Medical Marijuana Card
Veriheal has satisfied millions of patients nationwide by giving them access to these benefits
- Larger purchase limits
- Peace of mind
- Enhanced legal protection
- Access to higher potency strains
- Save up to 25% on cannabis purchases
- Skip the line at the dispensary
The Potential Role of Medical Cannabis in SPS
As we explore alternative treatments for Stiff Person Syndrome, medical cannabis stands out for its potential benefits. Research indicates that certain cannabinoids, particularly CBD (cannabidiol) and THC (tetrahydrocannabinol), effectively reduce muscle stiffness and spasms, common in SPS.
CBD is known for its pain-relieving and anti-inflammatory properties, while THC can help relax muscles and alleviate discomfort. Several studies and patient reports have highlighted the positive effects of these cannabinoids on SPS symptoms. For example, patients using medical cannabis have reported a significant decrease in the frequency and severity of their muscle spasms. Some have also noted an improvement in their overall mobility and a reduction in pain levels.
Both of these cannabinoids, THC and CBD, are available in a 1:1 mouth spray called Sativex. This is a pharmaceutical product that is approved in 29 foreign countries to help manage the moderate to severe specificity of multiple sclerosis (MS). While Sativex isn’t approved in the US yet, it is thought to potentially be a reasonable, experimental approach to SPS.
These findings suggest that cannabinoids, especially when used in specific ratios and dosages, could offer a valuable therapeutic option for managing SPS.
Case Study: Impact of Medical Cannabis on a PSPS Patient
In a recent 2020 study published in the Journal of Pain and Symptom Management, a 60-year-old woman with paraneoplastic stiff person syndrome (PSPS) faces a challenging medical journey. For years, she struggled with severe symptoms, including intense muscle spasms and debilitating pain, which significantly affected her way of life. Despite undergoing various conventional treatments, including numerous medications and therapies, she found little relief. Unfortunately, her condition continued to impact her quality of life severely, adding major depression and anxiety in the process.
In her quest for a solution, she decided to explore alternative treatments and turned to medical cannabis. This decision came after other therapies had limited success in managing her symptoms.
As a new medical cannabis patient, she took a combination of 1:1 THC:CBD tincture twice daily and CBD oil multiple times daily. She started with two drops of the 1:1 twice daily, and 1 drop of the CBD oil numerous times per day. She adjusted the number of drops until she found the dosages that worked for her.
After starting cannabis treatment, she observed a noticeable change. The frequency and intensity of her muscle spasms reduced substantially. She also reported an impressive decrease in her pain levels and medications. This improvement was a breakthrough, offering her a sense of relief and stability that she hadn’t experienced in years.
Her experience serves as a compelling case study on the potential benefits of medical cannabis for individuals with PSPS. It highlights how, in some situations, cannabis can be an effective alternative when traditional treatments fall short. It’s also consistent with a previous SPS case study from 2012, where a 40-year-old man also made effective use of 1:1 THC:CBD mouth spray.
Broader Implications and Future Directions
Diagnosing PSPS poses significant challenges, often leading to underdiagnosing and misdiagnoses. This demonstrates the need for better treatment strategies. The growing interest in medical cannabis offers new hope, particularly for managing neurological and cancer-related symptoms in PSPS.
As research continues, the potential of incorporating medical cannabis into PSPS treatment protocols becomes more promising. In the future, these new approaches could open additional avenues for effectively helping those struggling with this complex condition, paving the way for more comprehensive and tailored healthcare solutions.
The involvement of public figures like Celine Dion in raising awareness about rare disorders like Stiff Person Syndrome is invaluable. Their voices bring much-needed attention and support to these conditions, encouraging further research and understanding.
Author, Share & Comments