Multiple Sclerosis Patients Turn to Medical Marijuana for Help
- Relieving MS with Medical Cannabis
- Recommendations for Medical Marijuana and Multiple Sclerosis
- Typical MS Treatments
- MS and Medical Marijuana Considerations
- Understanding the Different Types of MS
More and more patients diagnosed with multiple sclerosis are turning to medical marijuana to ease their symptoms of neuropathy, chronic pain, and systemic inflammation. In fact, a 2014 survey by the North American Research Committee on Multiple Sclerosis (NARCOMS) found that out of 5,481 participants 47% were interested in using medical cannabis and its cannabinoids as part of their treatment (8).
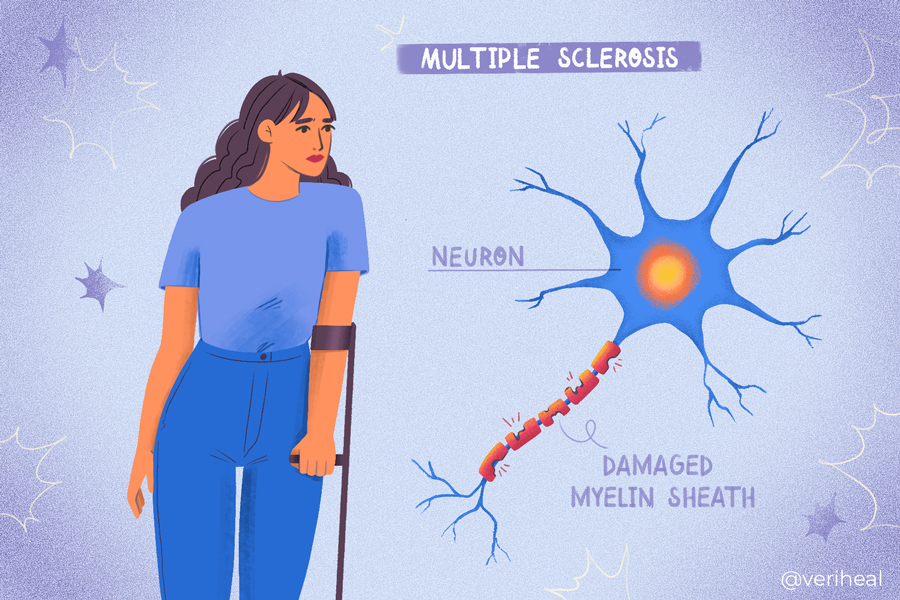
It is no wonder there is more interest in the medicinal properties of medical cannabis. There are over 100 different organic compounds that are found in cannabis with Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD) being the most well-known (3). When cannabis is ingested, it works by activating endocannabinoid receptors and other pathways. Endocannabinoids are fat-based neurotransmitters that work in your body and can activate and deactivate other neurotransmitters. THC is received by the CB1 and CB2 receptors of the endocannabinoid system. CBD weakly binds to both, but really works by increasing the levels of our endocannabinoids and hitting other receptors. This system of endocannabinoids and receptors is known as the endocannabinoid system.
Cannabis has been especially of interest to researchers who study multiple sclerosis (MS) as cannabis has immune-suppressive effects and is a neuroprotectant (22). CB1 receptors are in the central nervous system, which is the part of the nervous system that suffers from inflammation and nerve damage from MS. CB2 receptors are found on immune cells both within and outside the brain.
Researchers believe that cannabis can trigger apoptosis or cell death in myelin-specific T-cells (immune cells) that attack the nerves and cause inflammation (22). Other immune cell types, like MHCII, show reduced activity which further limits the targeting of myelin (neuron protective covering). These are positive responses for patients who have autoimmune conditions like MS where the body attacks itself.
In addition, CB1 and CB2 receptors increase the neurotransmitter anandamide (AEA) which has immunosuppressive effects on astrocytes, cells that make up 60-70% of brain cells in the central nervous system. Astrocytes secrete IL-6 when AEA is increased, which stimulates neuronal, or nerve cell growth (22).
A 2022 review in Biomedicines found some intriguing results regarding the use of cannabinoids in patients with multiple sclerosis (MS). This review found that several studies in humans and animals show strong evidence that cannabinoids may be able to slow the progression of MS. The data shows that cannabis can not only downregulate T-cells that are responsible for autoimmune attacks but they can also promote remyelination of nerves in certain situations (15). Remyelination, the rebuilding of the myelin on nerves, was specifically seen in Theiler’s murine encephalomyelitis virus-induced demyelinating disease (TMEV-IDD) in animals. Researchers are hopeful that this is also the case in MS, though there is still ongoing research about remyelination.
Relieving MS with Medical Cannabis
It is interesting to note that MS is considered a qualifying condition for medical marijuana in the majority of states that allow the use of cannabis for medical purposes. Please keep reading to find out how it may help with the major symptoms of multiple sclerosis. These symptoms often progress or worsen over time, causing issues with mobility and gait (20).
Chronic Pain
Chronic pain is one of the most well-known and documented symptoms that patients use medical cannabis for. There are several studies documenting the use of medical cannabis for various types of pain relief. Patients using medical cannabis for chronic pain also report improved mood and better sleep from both the use of marijuana itself as well as from reduced pain. According to the National MS Society, two-thirds of patients suffer from pain including headaches, nerve pain, back pain, spasticity, and trigeminal neuralgia (4).
Check out our page on chronic pain for more information on treatment options.
Spasticity
Spasticity, which is essentially severe and debilitating muscle spasms, is a common symptom in patients with MS. A 2003 study examined the use of cannabinoids (in the form of Cannador®) for spasticity in patients with multiple sclerosis. This study, known as the CAMS study, was a large-scale study with 630 participants who experienced spasticity, muscle stiffness, pain, and tremors. Patients were given capsules containing a 2:1 ratio of THC to CBD or, Delta-9-THC only, or a placebo (34). The study took place over 15 weeks.
The main study did not find that cannabis and its cannabinoids had a significant clinical impact using the Ashworth Scale (34). However, 61% of patients who participated in the study self-reported that Cannador® reduced their spasticity compared to 60% of patients who took THC only and 46% of patients on placebo. Despite its failure in initial clinical evaluations, researchers found that the objective improvements in spasticity and mobility reported by the patients make cannabis worth further evaluations.
However, a follow-up on the CAMS study 12 months after the main study did show a small impact on the Ashworth scale from patients on Cannador® and Delta-9-THC treatment. This could indicate that reversing the damage done by MS may take more time than previously thought. Longer and larger studies done over more than 12 months could demonstrate the further potential of cannabinoid treatment for MS.
Please check out our page on spasticity for more information about treating this symptom.
Neuropathy
Numbness, tingling, or burning sensations tend to plague patients with MS due to the demyelination and damage to the nerves. Medical marijuana has been shown by several studies to help patients suffering from nerve pain. Researchers believe that two areas of the brain that are responsible for processing pain signals in the central nervous system contain large amounts of CB1 receptors (30). These areas of the brain are the periaqueductal gray (PAG) and the rostral ventromedial medulla (RVM). This is important because it shows that CB1 receptors also play a role in nerves and pain signaling. Studies on MS and neuropathy are still lacking at this point.
Please check out our page on neuropathy for more information.
Tremors
Tremors are more than just bouts of shakiness for many patients with MS as they can be debilitating. A 2015 review examined the use of medical marijuana for treating tremors in patients with motor-related diseases such as MS, Parkinson’s disease, and Huntington’s disease (2). Researchers believe that the anecdotal evidence from MS patients about tremor reduction has been seen in newer studies in both animals and humans. They have also found that chronic or ongoing use of THC-rich extracts is effective in reducing both tremors and spasticity.
Recommendations for Medical Marijuana and Multiple Sclerosis
As reported in a National Institute of Health (NIH) research summit regarding cannabis and neuroscience (the field of study focusing on the brain and nerves), patients who are seeking to treat MS-related muscle spasticity and pain should consider cannabis strains higher in CBD or in equal parts to THC (26). THC is thought to reduce pain while CBD is known for its ability to reduce inflammation, which leads to demyelination and in some cases can also lead to chronic pain.
It is important to note, however, that as of 2020, the American Academy of Neurology (AAN) does not currently endorse the use of medical cannabis after publishing a systematic review in 2014 (4) (1). They found that studies examining smoked cannabis have not produced enough evidence to assess the effectiveness of medical marijuana on MS-related symptoms. Additional findings from the AAN include (4):
| Spasticity |
|
| Pain |
|
| Tremors |
|
| Urinary symptoms including urinary frequency & incontinence |
|
Typical MS Treatments
Unfortunately there is no cure for multiple sclerosis. There are a variety of treatments available to patients with multiple sclerosis, though not all patients find that these solutions provide enough pain relief for them and turn to other options such as medical cannabis. Traditional treatments typically focus on helping patients recover from attacks and relapses, manage symptoms, and slow the progression of the disease (19).
Corticosteroids and exchanging your blood plasma (the fluid portion of your blood) can help with relapses or attacks (19). Disease-modifying therapies (DMTs) in oral form may be prescribed for slowing the progression of the disease and include: fingolimod, siponimod, dimethyl fumarate, diroximel fumarate, and cladribine. Doctors may also prescribe injectable or infusion therapy medications including interferon beta medications, ocrelizumab, natalizumab, alemtuzumab, and glatiramer acetate. Many of these DMTs can cause severe side effects.
Physical therapy and antispasmodic agents are also important mainstays of treatment that can help with muscle spasms, muscle pain, walking, balance, and activities of daily living. MS can also be accompanied by other co-occurring conditions like depression, urinary frequency and incontinence, bowel problems, and sexual dysfunction. Psychological therapy and approved medication options exist to help address these related conditions. These commonly linked conditions can also greatly affect a patient’s quality of life and need approved treatments beyond what medical cannabis can offer.
Sativex for Multiple Sclerosis
Sativex (nabiximols) is a cannabis derivative prescription for MS treatment that is an oral spray. It contains a 1:1 ratio of CBD to THC. It is supposed to help with pain, fatigue, spasticity, bladder urgency, and mobility difficulties (5). Unfortunately, Sativex is not yet FDA-approved in the US but is approved in other countries like the UK, Spain, Germany, and Denmark. There are several studies supporting the efficacy of Sativex.
There are currently two synthetic cannabis-based prescriptions available in the United States, but they are not labeled to treat MS. Marinol (dronabinol) and Cesamet (nabilone) are both available in the form of oral capsules and are used for chemotherapy-induced nausea.
Using Cannador for MS
It is not yet available in the United States, but a medication called Cannador® is showing promise for patients with MS. Cannador is considered a natural cannabis extract and is a capsule containing a 2:1 ratio of THC and CBD (4). The CAMS study discussed above shows that there were a high fraction of patients who were able to get relief from their pain and spasticity (34).
A follow-up study to the CAMS study looked at the patients after utilizing the cannabis extract after 12 months (33). Patients who took the treatments containing Cannador or THC reported that these treatments were helpful in treating their symptoms. As opposed to the main study, this time a small effect on the Ashworth scale of spasticity was seen in patients treated with cannabinoids after 12 months. There were no safety concerns for participants for using THC or Cannador long-term.
MS and Medical Marijuana Considerations
It is important to consider that all medications, including medical cannabis, have both potential benefits and side effects. If you are experiencing seizures or epilepsy along with MS, it is crucial that you speak with your neurologist before using cannabis and it may increase your seizures or interact with other medications you may be taking. Using cannabis with certain medications such as tricyclic antidepressants and selective serotonin reuptake inhibitors may impact your liver’s ability to metabolize and utilize these medications (4).
Medical cannabis is not currently supported by the AAN and may cause additional issues in patients who have existing heart problems. Additionally, it can worsen cognitive function in some patients with MS (5).
Understanding the Different Types of MS
Even though multiple sclerosis is considered a disease of the central nervous system, including the brain and spinal cord, it can cause a variety of symptoms for those who have it. In some patients, symptoms are mild or may not be very noticeable. For others, it can be considered a disabling disease. Because of its nature, the signs and symptoms vary based on the amount of nerve damage as well as which nerves are affected (20). Although MS affects every patient differently, the main categories of multiple sclerosis are detailed out below.
Clinically Isolated Syndrome (CIS)
CIS is considered a precursor to MS, despite its classification as being one of the four disease courses of this disorder (6). It is considered the first episode of neurological symptoms a patient experiences and is caused by inflammation and demyelination of nerves and nerve cells in the central nervous system. Patients with this form of MS can experience a single (monofocal) symptom or several neurological symptoms (multifocal) at a time. These initial symptoms typically last at least 24 hours.
CIS is not a directly inherited condition (6). When it is detected and includes brain lesions identified on an MRI, the patient has a 60-80% chance of developing MS over time. Due to changes in diagnostic criteria in 2017, a patient with CIS may be able to be diagnosed with multiple sclerosis based on MRI results.
Relapsing-remitting Multiple Sclerosis (RRMS)
RRMS is considered the most common form of MS and includes 85% of patients diagnosed with this disorder (24). These patients experience periods of new symptoms and/or relapses that develop over days and weeks (20). Suddenly these symptoms seem to partially or completely improve without warning. These relapses in symptoms are usually followed by periods of remission that can last a few months or a few years. These symptom attacks are caused by inflammation attacks on the myelin membranes on nerve cells or the nerve fibers inside the myelin (the protective coating of the nerves).
Many patients with RRMS experience clearly defined neurological symptoms such as spasticity and neuropathy. Patients with RRMS are more likely to have brain lesions, inflammatory lesions, and spinal cord lesions than with other types of MS (24).
Secondary Progressive MS (SPMS)
At least 50% of patients with the relapsing form of MS end up developing progressively worsening symptoms within 10-20 years from the onset of the disease (20). These patients sometimes experience periods of remission, but not always. As the symptoms worsen, patients often experience issues with how they walk (gait) and their mobility. SPMS is usually diagnosed when the disease changes from gradual symptoms of inflammation to having actual nerve damage or nerve loss (27).
Primary Progressive Multiple Sclerosis (PPMS)
Some MS patients experience a gradual onset and a steady progression of neurological symptoms. This is known as primary progressive multiple sclerosis. Patients with PPMS do not experience relapses or remissions (23). They also tend to experience more issues with their mobility and have difficulty working, requiring more assistance with daily activities than those who have other forms of MS. This is interesting to note as patients with PPMS tend to have fewer brain lesions than those who suffer from the relapsing forms of MS.
Note: Veriheal does not intend to give this as professional medical advice. Do not attempt to self-diagnose, or prescribe treatment based on the information provided on this page. Always consult a physician before making any decision on the treatment of a medical condition.
1. American Academy of Neurology. (2020, September 9). AAN POSITION: USE OF MEDICAL CANNABIS FOR NEUROLOGIC DISORDERS. AAN. Retrieved March 29, 2022, from https://www.aan.com/advocacy/medical-cannabis-position-statement
2. Arjmand, S., Vaziri, Z., Behzadi, M., Abbassian, H., Stephens, G. J., & Shabani, M. (2015). Cannabinoids and Tremor Induced by Motor-related Disorders: Friend or Foe?. Neurotherapeutics: the journal of the American Society for Experimental NeuroTherapeutics, 12(4), 778–787. https://doi.org/10.1007/s13311-015-0367-5 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4604184/
3. Atakan Z. (2012). Cannabis, a complex plant: different compounds and different effects on individuals. Therapeutic advances in psychopharmacology, 2(6), 241–254. https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC3736954/
4. Cameron, M., & Rice, J. (2020). Cannabis for Multiple Sclerosis Symptoms. National MS Society. https://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Professionals/Cannabis-and-Multiple-Sclerosis.pdf
5. Cannabis. Cannabis – MS Society of Canada. (n.d.). Retrieved March 29, 2022, from https://mssociety.ca/hot-topics/cannabis
6. Clinically isolated syndrome (CIS). National Multiple Sclerosis Society. (n.d.). Retrieved March 29, 2022, from https://www.nationalmssociety.org/understanding-ms/what-is-ms/clinically-isolated-syndrome-
7. Cofield, S. S., Salter, A., Tyry, T., Crowe, C., Cutter, G. R., Fox, R. J., & Marrie, R. A. (2017). Perspectives on marijuana use and effectiveness: A survey of NARCOMS participants. Neurology. Clinical practice, 7(4), 333–343. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5648201/
8. Cofield, S. S., Salter, A., Tyry, T., Crowe, C., Cutter, G. R., Fox, R. J., & Marrie, R. A. (2017). Perspectives on marijuana use and effectiveness: A survey of NARCOMS participants. Neurology. Clinical practice, 7(4), 333–343. https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC5648201/
9. Collin, C., Davies, P., Mutiboko, I. K., Ratcliffe, S., & Sativex Spasticity in MS Study Group (2007). Randomized controlled trial of cannabis-based medicine in spasticity caused by multiple sclerosis. European journal of neurology, 14(3), 290–296. https://pubmed.ncbi.nlm.nih.gov/17355549/
10. Corey-Bloom, J., Wolfson, T., Gamst, A., Jin, S., Marcotte, T. D., Bentley, H., & Gouaux, B. (2012). Smoked cannabis for spasticity in multiple sclerosis: a randomized, placebo-controlled trial. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 184(10), 1143–1150. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3394820/
11. da Rovare, V. P., Magalhães, G., Jardini, G., Beraldo, M. L., Gameiro, M. O., Agarwal, A., Luvizutto, G. J., Paula-Ramos, L., Camargo, S., de Oliveira, L. D., Bazan, R., & El Dib, R. (2017). Cannabinoids for spasticity due to multiple sclerosis or paraplegia: A systematic review and meta-analysis of randomized clinical trials. Complementary therapies in medicine, 34, 170–185. https://pubmed.ncbi.nlm.nih.gov/28917371/
12. Fox, P., Bain, P. G., Glickman, S., Carroll, C., & Zajicek, J. (2004). The effect of cannabis on tremor in patients with multiple sclerosis. Neurology, 62(7), 1105–1109. https://n.neurology.org/content/62/7/1105
13. Gupta, S., Fellows, K., Weinstock-Guttman, B., Hagemeier, J., Zivadinov, R., & Ramanathan, M. (2019). Marijuana Use by Patients with Multiple Sclerosis. International Journal of MS Care, 21(2), 57–62. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6489434/
14. Hodges, C. (2016). Marijuana and Multiple sclerosis. Claire Hodges’ Account – Marijuana and Multiple sclerosis. Retrieved March 29, 2022, from http://rxmarijuana.com/Hodges.htm.
15. Longoria, V., Parcel, H., Toma, B., Minhas, A., & Zeine, R. (2022). Neurological benefits, clinical challenges, and Neuropathologic promise of medical marijuana: A systematic review of cannabinoid effects in multiple sclerosis and experimental models of Demyelination. Biomedicines, 10(3), 539. https://www.mdpi.com/2227-9059/10/3/539/htm
16. Maayah, Z.H., Takahara, S., Ferdaoussi, M. et al. The anti-inflammatory and analgesic effects of formulated full-spectrum cannabis extract in the treatment of neuropathic pain associated with multiple sclerosis. Inflamm. Res. 69, 549–558 (2020). https://link.springer.com/article/10.1007/s00011-020-01341-1
17. Malfitano AM, Matarese G, Bifulco M. From cannabis to endocannabinoids in multiple sclerosis: a paradigm of central nervous system autoimmune diseases. Curr Drug Targets CNS Neurol Disord. 2005 Dec;4(6):667-75. https://pubmed.ncbi.nlm.nih.gov/16375684/
18. Malfitano AM, Proto MC, Bifulco M. Cannabinoids in the management of spasticity associated with multiple sclerosis. Neuropsychiatr Dis Treat. 2008 Oct;4(5):847-53. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2626929/
19. Mayo Foundation for Medical Education and Research. (2022, January 7). Multiple sclerosis- Diagnosis & Treatment. Mayo Clinic. Retrieved March 29, 2022, from https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/diagnosis-treatment/drc-20350274
20. Mayo Foundation for Medical Education and Research. (2022, January 7). Multiple Sclerosis- Symptoms & Causes. Mayo Clinic. Retrieved March 29, 2022, from https://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/symptoms-causes/syc-20350269
21. Multiple sclerosis. NORML. (2021, September 21). Retrieved March 29, 2022, from https://norml.org/marijuana/library/recent-medical-marijuana-research/multiple-sclerosis/
22. Nagarkatti, P., Pandey, R., Rieder, S. A., Hegde, V. L., & Nagarkatti, M. (2009). Cannabinoids as novel anti-inflammatory drugs. Future medicinal chemistry, 1(7), 1333–1349. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2828614/
23. Primary progressive MS (ppms). National Multiple Sclerosis Society. (n.d.). Retrieved March 29, 2022, from https://www.nationalmssociety.org/What-is-MS/Types-of-MS/Primary-progressive-MS
24. Relapsing-remitting MS (RRMS). National Multiple Sclerosis Society. (n.d.). Retrieved March 29, 2022, from https://www.nationalmssociety.org/What-is-MS/Types-of-MS/Relapsing-remitting-MS
25. Rizzo, M. A., Hadjimichael, O. C., Preiningerova, J., & Vollmer, T. L. (2004). Prevalence and treatment of spasticity reported by multiple sclerosis patients. Multiple Sclerosis Journal, 10(5), 589–595. https://europepmc.org/article/MED/15471378
26. Rudroff, T., & Honce, J. M. (2017). Cannabis and Multiple Sclerosis-The Way Forward. Frontiers in neurology, 8, 299. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5481305/
27. Secondary Progressive MS (SPMS). National Multiple Sclerosis Society. (n.d.). Retrieved March 29, 2022, from https://www.nationalmssociety.org/What-is-MS/Types-of-MS/Secondary-progressive-MS
28. Urits, I., Adamian, L., Fiocchi, J., Hoyt, D., Ernst, C., Kaye, A. D., & Viswanath, O. (2019). Advances in the Understanding and Management of Chronic Pain in Multiple Sclerosis: a Comprehensive Review. Current pain and headache reports, 23(8), 59. https://pubmed.ncbi.nlm.nih.gov/31342191/
29. Ware, M. A., Wang, T., Shapiro, S., Collet, J.-P., Boulanger, A., Esdaile, J. M., Gordon, A., Lynch, M., Moulin, D. E., & O’Connell, C. (2015). Cannabis for the management of Pain: Assessment of safety study (Compass). The Journal of Pain, 16(12), 1233–1242. https://www.jpain.org/article/S1526-5900(15)00837-8/fulltext
30. Wilsey, B., Marcotte, T., Tsodikov, A., Millman, J., Bentley, H., Gouaux, B., & Fishman, S. (2008). A randomized, placebo-controlled, crossover trial of cannabis cigarettes in neuropathic pain. The journal of pain, 9(6), 506–521. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4968043/
31. Whiting, P. F., Wolff, R. F., Deshpande, S., Di Nisio, M., Duffy, S., Hernandez, A. V., Keurentjes, J. C., Lang, S., Misso, K., Ryder, S., Schmidlkofer, S., Westwood, M., & Kleijnen, J. (2015). Cannabinoids for Medical Use: A Systematic Review and Meta-analysis. JAMA, 313(24), 2456–2473. https://pubmed.ncbi.nlm.nih.gov/26103030/
32. Zajicek, J. P., Sanders, H. P., Wright, D. E., Vickery, P. J., Ingram, W. M., Reilly, S. M., Nunn, A. J., Teare, L. J., Fox, P. J., & Thompson, A. J. (2005). Cannabinoids in multiple sclerosis (CAMS) study: safety and efficacy data for 12 months follow up. Journal of neurology, neurosurgery, and psychiatry, 76(12), 1664–1669. https://pubmed.ncbi.nlm.nih.gov/16291891/
33. Zajicek JP, Sanders HP, Wright DE, et al. Cannabinoids in multiple sclerosis (CAMS) study: safety and efficacy data for 12 months follow up.Journal of Neurology, Neurosurgery & Psychiatry 2005;76:1664-1669. https://jnnp.bmj.com/content/76/12/1664
34. Zajicek, J., Fox, P., Sanders, H., Wright, D., Vickery, J., Nunn, A., Thompson, A., & UK MS Research Group (2003). Cannabinoids for treatment of spasticity and other symptoms related to multiple sclerosis (CAMS study): multicentre randomised placebo-controlled trial. Lancet (London, England), 362(9395), 1517–1526. https://pubmed.ncbi.nlm.nih.gov/14615106/