Phantom Pain and Medical Cannabis Treatment
Many states allow patients experiencing chronic pain and neuropathy to participate in medical marijuana programs, giving patients access to the benefits of medical cannabis.
Phantom limb pain is considered both neuropathic pain and chronic pain that occurs after amputation or loss of a body part. Though there is not a lot of research specifically on phantom limb pain and cannabis, many researchers believe that it could be helpful to patients.
- Can Medical Cannabis Help Phantom Limb Pain
- What Does the Research Say About Phantom Limb Pain & Cannabis?
- Thoughts to Consider Regarding Cannabis Treatments
- What is Phantom Limb Pain?
- More About Phantom Limb Pain
Can Medical Cannabis Help Phantom Limb Pain?
Phantom limb pain is closely associated with referred, residual, and chronic pain. Compounds in the cannabis plant can interact with receptors in the body that manage the perception of these types of pain.
Though research about the impact of cannabis on phantom limb pain is in its early stages, plenty of research suggests that cannabis can help with pain management post-amputation.
Cannabis contains over 120 different naturally occurring compounds called cannabinoids. The best-known cannabinoids include Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD). When cannabinoids are smoked or consumed, they activate cannabinoid receptors CB1 and CB2. These receptors help increase or decrease the levels of fatty-based neurotransmitters in the body called endocannabinoids. This system called the endocannabinoid system (ECS) is responsible for controlling how our body perceives pain, relays inflammation, and fights off infections.
Cannabinoids like CBD, cannabigerol (CBG), and other minor cannabinoids can also activate other anti-inflammatory and analgesic receptors in the body including serotonin, GPR55, and TRP receptors as part of the greater endocannabinoidome (eCBome) (38).
Researchers believe that nerve pain is partially modulated by a specific serotonin receptor called 5-HT2A (7). Pain is also modulated through N-methyl-D-aspartate (NDMA) activation, which helps relieve pain. Opioid medications activate both 5-HT2A and NDMA but can contribute to intensifying central sensitization by activating pronociceptive, or pro-pain pathways. This can intensify pain because the body is hypersensitive to the activated pain receptors.
Cannabis also activates these receptors, especially 5-HT1A by THC, CBD, cannabidiolic acid (CBDA), and CBG (38). When THC and CBD interact with 5-HT2A signaling to these receptors is downregulated instead of increased. This is the opposite of how opioids work on these receptors. Researchers believe that this downregulation helps suppress inflammation and can help changes in mood that also contribute to chronic pain (7).
What Does The Research Say About Phantom Limb Pain & Cannabis?
A 2018 review from the Cleveland Clinic stated that peripheral neuropathy significantly worsens a patient’s quality of life and function (19). It also can cause emotional, cognitive, and functional issues for those patients. Many doctors consider phantom limb pain a type of peripheral neuropathy and cite a lack of treatment options for this type of pain.
A 2014 study found that vaporized cannabis given at low doses can help relieve peripheral neuropathic pain. This study was a placebo and double-blind trial that tested vaporized cannabis with the THC removed as well as a range of vaporized cannabis containing 1.29% to 3.53% THC, labeled as low-dose and medium-dose respectively (40).
A total of 39 participants received the medications for the study. The average reported pain intensity before and after consuming the study cannabis was evaluated. Previously, the authors had conducted a similar study in 2008 comparing placebo, 3.5% THC, and 7% THC. The new lower dose (1.29%) was introduced in the follow-up 2014 study (40).
This study found that low-dose (1.29%) and medium-dose (3.53%) THC provided equal pain relief when evaluated. Pain reduction results were measured throughout the trial at the same time intervals. It also found that the 1.29% had minimal effect on cognitive function tests while helping improve pain (40). The low dose of cannabis was able to reduce the participant’s pain by 30%, significantly greater than the placebo and comparable to current neuropathic treatment options.
This study shows promising results, but researchers cited the ability to mask cannabis versus placebo in terms of mind-altering effects as a problem with the study design. However, it also highlights a clinical advantage which is that even low-dose THC (1.29%) cannabis products may significantly reduce neuropathic pain with less compromise of cognitive function or other undesired side effects. This may help patients achieve less pain associated with their missing limb while minimizing the impact on daily functioning.
Please check out our page on neuropathy for more information and research.
Cannabinoids and Ocular Phantom Limb Pain
A 2022 review from Biomedicine & Pharmacotherapy suggests that cannabinoid-based therapies for ocular pain should be developed and studied (33). This review cites that cannabis has been shown to both decrease inflammation and chronic pain, as well as neuropathic pain. This is important in terms of treating eye pain as it often has a mix of causes. It is also important to know that phantom eye pain itself is an underestimated complication of having an eye amputation.
Unfortunately because of the lack of research in this area, medical cannabis cannot be formally recommended at this time based on clinical research on cannabinoids and eye pain. This is because there isn’t really much research in this area. However, researchers speculate that based on how cannabis helps in other types of pain, it may potentially be useful (33).
Thoughts to Consider Regarding Cannabis Treatments
It is important to note that research levels of THC content in cannabis often differ from what is available from dispensaries. According to the Cleveland Clinic, dispensary-available preparations may contain much higher THC and upwards of 23 times more cannabinol (CBN) than the government-supplied cannabis approved for research use (19). This means that practical and tolerability results may vary from available clinical data.
Another important note is that it is crucial to speak with your healthcare provider who may be prescribing medical cannabis to you about any other health problems, pain medicines, or medications you may be taking. For example, cannabis use may not be indicated in patients who are experiencing seizures, critical illness, pregnancy, or heart issues.
What is Phantom Limb Pain?
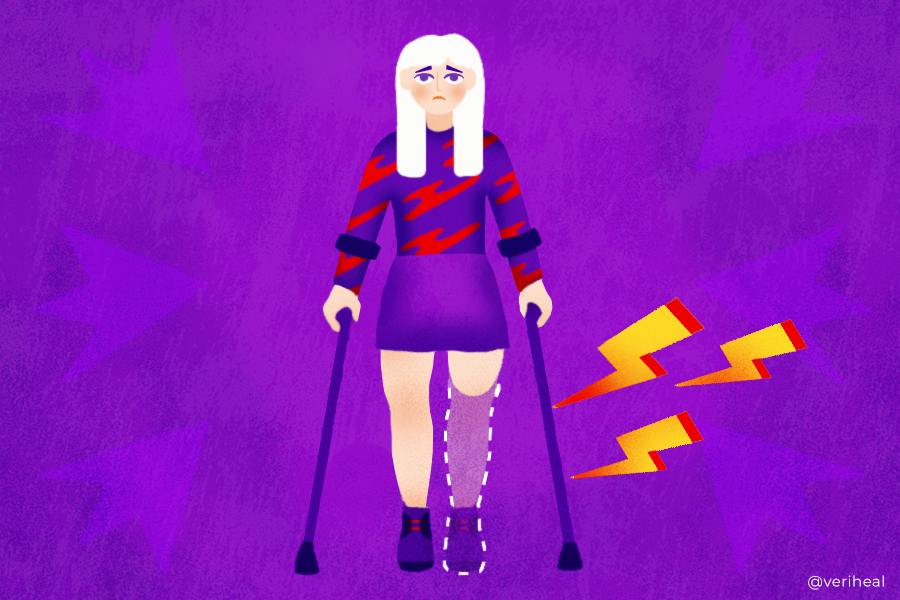
Phantom limb pain often occurs after limb amputation (28). Amputees with phantom limb pain report that their symptoms are coming from the missing body part, though that body part no longer has sensation.
Many patients report the following sensations regarding their pain (28):
- Throbbing
- Cramping
- Burning
- Sharp shooting or stabbing pain
- Tingling pain or pins and needles
- Electric shocks
Phantom limb pain is often considered both a form of chronic pain as well as neuropathy. This debilitating condition can be long-lasting without the proper treatments. It is believed to be caused by physical and psychological factors (2), increasing its difficulty to treat.
Specific factors include changes in key areas like the peripheral nerves, the brain, and the spinal cord, as well as psychological changes like depression, anxiety, and increased stress (11). Many patients experience phantom limb pain intermittently, and it is more common in upper-extremity amputations and lower-extremity limb loss. It is often experienced in the form of attacks that can last anywhere from a few seconds to several hours.
There are several different areas of phantom limb pain patients can experience including phantom pain in the limbs, phantom breast pain, and phantom eye pain.
These types of pain are considered a type of nerve pain, or neuropathy. They can lead to chronic pain in patients who are experiencing them.
More About Phantom Limb Pain
Phantom limb pain often occurs when a limb or other body part has been removed (28). Patients with phantom limb pain report that their symptoms are coming from the amputated limb, though that body part no longer has sensation. Patients can experience this type of pain in the following parts of the body (28):
- Arms, hands, legs, or feet
- Eyes
- Teeth
- Nose
- Tongue
- Breasts
- Penis
- Parts of the intestinal tract
Phantom limb pain is often considered both a form of chronic pain as well as neuropathy. It can be long-lasting without the proper treatments. It is believed to be caused by a combination of physical and psychological factors (2), increasing its difficulty to treat. Specific factors include changes in key areas like the peripheral nerves, the brain, and the spinal cord, as well as psychological changes like depression, anxiety, and increased stress (11). Many patients experience phantom limb pain intermittently, and it is more common in upper extremity amputations and lower extremities. It is often experienced in the form of attacks that can last anywhere from a few seconds to several hours.
Many patients report the following sensations regarding their pain (28):
- Throbbing
- Cramping
- Burning
- Sharp shooting or stabbing pain
- Tingling pain or pins and needles
- Electric shocks
Phantom Limb Pain vs Referred Pain
It’s easy to confuse phantom limb pain and referred pain after accidents or surgeries that remove body parts. Phantom limb pain occurs in parts of the body that are no longer there. Referred pain is a type of pain that is experienced in one body part when a different body part is experiencing pain or injury (30).
Referred pain happens because of how the nerves in the body are connected and how they sense pain. It often happens after gallbladder surgery where the pain is felt instead in the shoulder. The sensation of a brain freeze is also considered referred pain, as the pain is actually occurring in the mouth and throat instead of the brain.
What is Residual Limb Pain?
Residual limb pain is a type of pain felt in the remaining part of a limb that occurs after amputation (31). It can start often in the first week after the amputation has taken place, and it can also last longer than the normal time periods of recovery. This type of pain usually is not severe and it is different from phantom limb pain as patients feel it in the remaining limb. Patients report that it feels like pressing, throbbing, burning squeezing, or stabbing pain (11).
Residual limb pain has been shown to occur in at least 50% of patients who are experiencing phantom limb pain (31). Unlike phantom limb pain, researchers have ideas on what causes it, including (31):
- Problems in the bone or soft tissues of the limb
- Infection
- Poor blood supply to the limb
- A tumor
- Problems with the fit or use of a prosthesis
Note: Veriheal does not intend to give this as professional medical advice. Do not attempt to self-diagnose or prescribe treatment based on the information provided on this page. Always consult a physician before making any decision on the treatment of a medical condition.
1. Alviar, M. J. M., Hale, T., & Lim-Dungca, M. (2016). Pharmacologic interventions for treating phantom limb pain. Cochrane Database of Systematic Reviews, 10. https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD006380.pub3/full
2. Andreotti, A. M., Goiato, M. C., Pellizzer, E. P., Pesqueira, A. A., Guiotti, A. M., Gennari-Filho, H., & dos Santos, D. M. (2014). Phantom Eye Syndrome: A Review of the Literature. The Scientific World Journal, 2014, 686493. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4273592/
3. Bridges, D., Thompson, S. W. N., & Rice, A. S. C. (2001). Mechanisms of neuropathic pain. British Journal of Anaesthesia, 87(1), 12–26. https://www.bjanaesthesia.org/article/S0007-0912(17)36340-7/fulltext
4. Collins, K. L., Russell, H. G., Schumacher, P. J., Robinson-Freeman, K. E., O’Conor, E. C., Gibney, K. D., Yambem, O., Dykes, R. W., Waters, R. S., & Tsao, J. W. (2018). A review of current theories and treatments for phantom limb pain. The Journal of Clinical Investigation, 128(6), 2168–2176. https://www.jci.org/articles/view/94003
5. Culp, C. J., & Abdi, S. (2022). Current Understanding of Phantom Pain and its Treatment. Pain Physician, 25(7), E941–E957. http://www.scopus.com/inward/record.url?scp=85140487673&partnerID=8YFLogxK
6. Dijkstra, P. U., Geertzen, J. H. B., Stewart, R., & Schans, C. P. van der. (2002). Phantom pain and risk factors: A multivariate analysis. Journal of Pain and Symptom Management, 24(6), 578–585. https://www.jpsmjournal.com/article/S0885-3924(02)00538-9/fulltext
7. Edinoff, A. N., Fort, J. M., Singh, C., Wagner, S. E., Rodriguez, J. R., Johnson, C. A., Cornett, E. M., Murnane, K. S., Kaye, A. M., & Kaye, A. D. (2022). Alternative Options for Complex, Recurrent Pain States Using Cannabinoids, Psilocybin, and Ketamine: A Narrative Review of Clinical Evidence. Neurology International, 14(2), Article 2. https://www.mdpi.com/2035-8377/14/2/35
8. Erlenwein, J., Diers, M., Ernst, J., Schulz, F., & Petzke, F. (2021). Clinical updates on phantom limb pain. Pain Reports, 6(1), e888. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7813551/
9. Flor, H. (2008). Maladaptive plasticity, memory for pain and phantom limb pain: Review and suggestions for new therapies. Expert Review of Neurotherapeutics, 8(5), 809–818. https://www.tandfonline.com/doi/full/10.1586/14737175.8.5.809
10. Gutierrez, T., & Hohmann, A. G. (2011). Cannabinoids for the treatment of neuropathic pain: Are they safe and effective? Future Neurology, 6(2), 129–133. https://www.futuremedicine.com/doi/full/10.2217/fnl.11.6
11. Hanyu-Deutmeyer, A. A., Cascella, M., & Varacallo, M. (2022). Phantom Limb Pain. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448188/
12. Häuser, W., Finn, D. P., Kalso, E., Krcevski-Skvarc, N., Kress, H.-G., Morlion, B., Perrot, S., Schäfer, M., Wells, C., & Brill, S. (2018). European Pain Federation (EFIC) position paper on appropriate use of cannabis-based medicines and medical cannabis for chronic pain management. European Journal of Pain, 22(9), 1547–1564. https://onlinelibrary.wiley.com/doi/abs/10.1002/ejp.1297
13. Helyes, Z., & Botz, B. (2013). Neuropathic and phantom pain. Influencing pain. http://rgdoi.net/10.13140/RG.2.1.2085.9049
14. Hirsch, E., Gierlich, J., Glants, E., Sheikh, T., Duran, D., & Krishna, R. (2019). Rebound Pain in a Patient Taking Medical Marijuana for Phantom Limb Syndrome (P3.9-054). Neurology, 92(15 Supplement). https://n.neurology.org/content/92/15_Supplement/P3.9-054
15. Kuner, R., & Flor, H. (2017). Structural plasticity and reorganisation in chronic pain. Nature Reviews Neuroscience, 18(1), Article 1. https://www.nature.com/articles/nrn.2016.162
16. Managing Phantom Pain. (n.d.). Amputee Coalition. Retrieved March 1, 2023, from https://www.amputee-coalition.org/limb-loss-resource-center/resources-for-pain-management/managing-phantom-pain/
17. Manzanares, J., Julian, M., & Carrascosa, A. (2006). Role of the Cannabinoid System in Pain Control and Therapeutic Implications for the Management of Acute and Chronic Pain Episodes. Current Neuropharmacology, 4(3), 239–257. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2430692/
18. McDonough, P., McKenna, J. P., McCreary, C., & Downer, E. J. (2014). Neuropathic orofacial pain: Cannabinoids as a therapeutic avenue. The International Journal of Biochemistry & Cell Biology, 55, 72–78. https://www.sciencedirect.com/science/article/pii/S1357272514002581
19. Modesto-Lowe, V., Bojka, R., & Alvarado, C. (2018). Cannabis for peripheral neuropathy: The good, the bad, and the unknown. Cleveland Clinic Journal of Medicine, 85(12), 943–949. https://www.ccjm.org/content/85/12/943
20. Moore, R. A., Fisher, E., Finn, D. P., Finnerup, N. B., Gilron, I., Haroutounian, S., Krane, E., Rice, A. S. C., Rowbotham, M., Wallace, M., & Eccleston, C. (2021). Cannabinoids, cannabis, and cannabis-based medicines for pain management: An overview of systematic reviews. PAIN, 162, S67. https://journals.lww.com/pain/fulltext/2021/07001/cannabinoids,_cannabis,_and_cannabis_based.6.aspx
21. Mücke, M., Weier, M., Carter, C., Copeland, J., Degenhardt, L., Cuhls, H., Radbruch, L., Häuser, W., & Conrad, R. (2018). Systematic review and meta‐analysis of cannabinoids in palliative medicine. Journal of Cachexia, Sarcopenia and Muscle, 9(2), 220–234. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5879974/
22. Nortvedt, F., & Engelsrud, G. (2014). “Imprisoned” in pain: Analyzing personal experiences of phantom pain. Medicine, Health Care, and Philosophy, 17(4), 599–608. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4182588/
23. Oana, A. C., Horia, P., Laurentiu, C., Anca, B., & Ion, F. (2008). Recent data on cannabinoids and their pharmacological implications in neuropathic pain. Journal of Medicine and Life, 1(4), 365–375. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5654208/
24. Odonkor, C. A., AlFarra, T., Adekoya, P., Orhurhu, V., Rodríguez, T., Sottosanti, E., & Kaye, A. D. (2022). Dorsal Column Stimulation and Cannabinoids in the Treatment of Chronic Nociceptive and Neuropathic Pain: A Review of the Clinical and Pre-clinical Data. Current Pain and Headache Reports, 26(2), 103–118. https://link.springer.com/article/10.1007/s11916-022-01008-y
25. Pantoja-Ruiz, C., Restrepo-Jimenez, P., Castañeda-Cardona, C., Ferreirós, A., & Rosselli, D. (2022). Cannabis and pain: A scoping review. Brazilian Journal of Anesthesiology (English Edition), 72(1), 142–151. https://www.sciencedirect.com/science/article/pii/S0104001421002748
26. Phantom limb pain: MedlinePlus Medical Encyclopedia. (n.d.). Retrieved March 1, 2023, from https://medlineplus.gov/ency/patientinstructions/000050.htm
27. Phantom Limb Pain—Physiopedia. (n.d.). Retrieved March 1, 2023, from https://www.physio-pedia.com/Phantom_Limb_Pain
28. Phantom Pain Symptoms, Causes, Medications, and Treatments. (2022, May 20). Healthline. https://www.healthline.com/health/phantom-pain
29. Ramesh, Shukla, N. K., & Bhatnagar, S. (2009). Phantom Breast Syndrome. Indian Journal of Palliative Care, 15(2), 103–107. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902108/
30. Referred Pain: Common Areas and What It Means. (2019, October 29). Healthline. https://www.healthline.com/health/pain-relief/referred-pain
31. Residual limb pain—Symptoms and causes. (n.d.). Mayo Clinic. Retrieved March 1, 2023, from https://www.mayoclinic.org/diseases-conditions/residual-limb-pain/symptoms-causes/syc-20541403
32. Russo, E. B. (2013). Cannabis and Cannabinoids: Pharmacology, Toxicology, and Therapeutic Potential.
33. Routledge, Scuteri, D., Rombolà, L., Hamamura, K., Sakurada, T., Watanabe, C., Sakurada, S., Guida, F., Boccella, S., Maione, S., Gallo Afflitto, G., Nucci, C., Tonin, P., Bagetta, G., & Corasaniti, M. T. (2022). Is there a rational basis for cannabinoids research and development in ocular pain therapy? A systematic review of preclinical evidence. Biomedicine & Pharmacotherapy, 146, 112505. https://www.sciencedirect.com/science/article/pii/S0753332221012919
34. Sainsbury, B., Bloxham, J., Pour, M. H., Padilla, M., & Enciso, R. (2021). Efficacy of cannabis-based medications compared to placebo for the treatment of chronic neuropathic pain: a systematic review with meta-analysis. Journal of dental anesthesia and pain medicine, 21(6), 479–506. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8637910/
35. Skrabek, R., & Galimova, L. (2007). (739/Paper 318): A randomized double-blind placebo controlled trial assessing the effect of the oral cannabinoid nabilone on pain and quality of life in patients with fibromyalgia. The Journal of Pain, 8(4), S35. https://www.jpain.org/article/S1526-5900(07)00231-3/fulltext
36. Subedi, B., & Grossberg, G. T. (2011). Phantom Limb Pain: Mechanisms and Treatment Approaches. Pain Research and Treatment, 2011, 864605. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3198614/
37. Thaler, A., Gupta, A., & Cohen, S. P. (2011). Cannabinoids for Pain Management. Chronic Pain and Addiction, 30, 125–138. https://www.karger.com/Article/FullText/324070
38. Walsh, K. B., McKinney, A. E., & Holmes, A. E. (2021). Minor Cannabinoids: Biosynthesis, Molecular Pharmacology and Potential Therapeutic Uses. Frontiers in pharmacology, 12, 777804. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8669157/
39. Welch, S. P. (2009). Interaction of the cannabinoid and opioid systems in the modulation of nociception. International Review of Psychiatry, 21(2), 143–151. https://www.tandfonline.com/doi/full/10.1080/09540260902782794
40. Wilsey, B., Marcotte, T. D., Deutsch, R., Gouaux, B., Sakai, S., & Donaghe, H. (2013). Low Dose Vaporized Cannabis Significantly Improves Neuropathic Pain. The Journal of Pain : Official Journal of the American Pain Society, 14(2), 136–148. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3566631/
41. Wolf, J., Urits, I., Orhurhu, V., Peck, J., Orhurhu, M. S., Giacomazzi, S., Smoots, D., Piermarini, C., Manchikanti, L., Kaye, A. D., Kaye, R. J., & Viswanath, O. (2020). The Role of the Cannabinoid System in Pain Control: Basic and Clinical Implications. Current Pain and Headache Reports, 24(7), 35. https://link.springer.com/article/10.1007/s11916-020-00873-9
42. Yaputra, F., & Widyadharma, I. (2018). Management of Phantom Limb Pain: A Review. International Journal of Medical Reviews and Case Reports, 1. http://www.ejmanager.com/fulltextpdf.php?mno=294990