Medical Marijuana & Pulmonary Fibrosis: Can it Help?
Medical cannabis and its cannabinoids have been shown to improve the severity of pulmonary fibrosis.
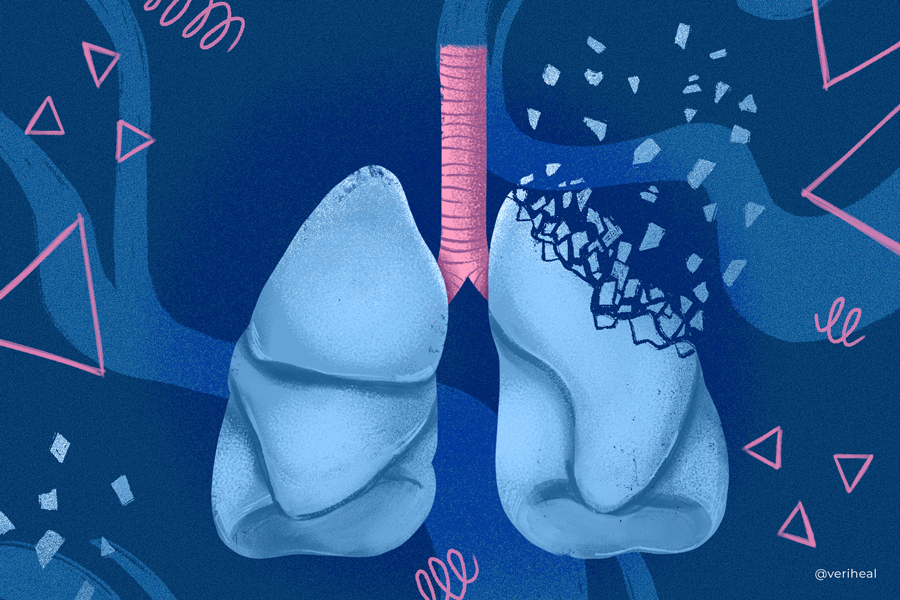
Pulmonary fibrosis is considered both a complication and a type of lung disease. Patients with pulmonary fibrosis may notice shortness of breath upon exercising and a chronic dry cough. This condition occurs when the lung tissue is scarred and develops fibrotic, or scar, tissue. Scientists are currently working on researching pulmonary fibrosis treatments as it can be a debilitating, progressive lung issue.
Many researchers believe that the endocannabinoid system (ECS) in our bodies may hold the key to treating pulmonary fibrosis. Cannabis contains over 120 naturally-occurring compounds called cannabinoids. When cannabis is ingested, the body can use the medicinal properties of cannabinoids including Δ9-tetrahydrocannabinol (THC), cannabidiol (CBD), and cannabigerol (CBG).
Medical cannabis activates various receptors that are part of the ECS including cannabinoid receptors CB1 & CB2, and receptors outside the ECS like peroxisome proliferator-activated receptors (PPARs). These receptors can increase or decrease the levels of fatty-based neurotransmitters called endocannabinoids. Endocannabinoids are important as they send messages to the body that controls how we feel pain, reduce inflammation, and maintain our appetites.
How Does Cannabis Help Pulmonary Fibrosis?
Thickening and scarring of tissues, a condition called fibrosis, can occur in many different places in our bodies. When this occurs in the lungs, it is called pulmonary fibrosis. When the body is injured, such as from inhaling sawdust, the immune system sends inflammatory cells called fibroblasts to repair the affected tissues (33).
The process of tissue repair, or wound healing consists of several steps. Fibroblasts along with macrophages and other inflammatory cells work to stop the damage or bleeding through hemostasis initially. Think of the scab that forms on top of a cut- this is the same process.
The body then continues to repair the lungs with inflammation by sending inflammatory cells to heal the tissue. Sometimes the body gets confused and never stops sending the inflammatory cells to the lungs, leading to scarring and pain for patients (33).
CB1 and CB2 receptors are expressed naturally in inflammatory fibroblasts and macrophages (33). CB1 receptors are known to be activated by THC while CB2 receptors work with the cannabinoid CBD.
When CBD activates cannabinoid receptors in inflammatory cells, it triggers the cells to die in a process called apoptosis. After the fibroblasts and macrophages die, they stop targeting the tissues that are chronically inflamed. This stops the inflammation cycle in the lungs and can slow the development of fibrosis in the lungs, leading to improvements in patients with pulmonary fibrosis.
Interestingly, the process of apoptosis in the lungs was also found to slow the progression of COVID-19 when the virus was in its original state in 2020 (40). Many COVID-19 patients suffered from pulmonary fibrosis as a result of the virus.
Recommendations for Pulmonary Fibrosis & Medical Cannabis
Medical cannabis shows potential in treating inflammatory conditions without the downsides of nonsteroidal anti-inflammatory drugs (NSAIDs), a mainstay of treatment options for patients who struggle with breathing issues and pain from pulmonary fibrosis (42).
Anti-inflammatory drugs have been shown to have little benefit to patients with pulmonary fibrosis, bringing up the question of if scarring and fibroids are actually caused by inflammation (12).
Fundacion Canna recommends that patients who are looking to treat pulmonary fibrosis begin cannabinoid treatments with 100-300mg of CBD. This is because of CBD’s role in modulating levels of anandamide, an endocannabinoid responsible for modulating a variety of processes in the body (12).
Additionally, cannabinoids have been shown to hold promise for respiratory health in the following conditions:
A Note on Medical Cannabis & Pulmonary Fibrosis
It is important to note that research in this area is still being conducted in order to see if the benefits outweigh the potential lung damage that can be caused by smoking medical cannabis.
For patients who are concerned about further lung damage, other medical marijuana options are available including edibles, tinctures, and oils.
Smoking cannabis, along with tobacco has been shown to be detrimental to lung health, and the choice to do so must not be taken lightly.
Pulmonary Fibrosis & Cannabis Research
A 2017 research study set out to test what happens when the CB2 receptor is activated (8). This study examined lung tissue samples and CB2 activation in living mice. Pulmonary fibrosis was induced in these mice with bleomycin, an anticancer drug, after 21 days of treatment. The tissue samples of the mice were then examined.
Researchers found that pulmonary fibrosis was decreased after exposure to a CB2 receptor agonist JWH133 (8). This occurred through the activation of the CB2 receptor in fibroblasts, a proinflammatory cell found in the lungs. Fibroblast levels increased along with their movement which decreased lung damage (8).
Because pulmonary fibrosis was induced in mice in this study, researchers were unable to see the results in the early stages of the symptoms (8). This study also didn’t use full-spectrum, plant-based medical cannabis, but it does show that the endocannabinoid system is a strong target for treating pulmonary fibrosis.
A different animal study from 2020 examined the use of NCMB-1, a compound containing hemp-extracted CBD in African green monkeys with lung fibrosis (41). African green monkeys were chosen for this experiment due to the similarity in lung tissues to humans. The monkeys were divided into a control group and groups that received 50μL of undiluted, 5x dilution, and 25x dilution NCMB-1.
After pulmonary fibrosis was induced and NCMB-1 was administered twice daily in bananas, the monkeys were evaluated for lung tidal volume, inspiratory flow rate, and respiration rate (41). The respiration rates in the monkeys who received 5x dilution and undiluted NCMB-1 showed increases in respiratory rates compared to the control group. Tidal flow volume and inspiratory flow rate were also increased in monkeys that received the 5x dilution compound.
This research is promising in that CBD has the potential to increase respiration rates in humans as well. Between increasing breathing rates and its ability to reduce fibrosis, medical cannabis has the potential to improve the quality of life in patients with lung issues.
Symptoms & Types of Pulmonary Fibrosis
Pulmonary fibrosis can occur in several different lung diseases or the cause may be unknown. Fibrosis in the lungs occurs when the tissue becomes inflamed and begins to scar. This leads to the development of scar tissue, or fibrosis, that can stiffen the tissues in the lungs.
Because pulmonary fibrosis or scarring of the lung tissue can occur in many different lung diseases, your exact symptoms may vary but can include (1):
- Fast breathing rate
- Dry, non-productive cough (21)
- Fatigue (21)
- Hypoxia, or lack of oxygen
- Shortness of breath at rest or with activity (15)
- Crackling in the lungs
- Scleroderma and other skin changes
- Sjogren’s syndrome
- Wheezing
- Raynaud’s phenomenon
- Muscle weakness & joint pain
- Neuropathy
- Clubbing of fingers and toes (21)
Idiopathic Pulmonary Fibrosis
Idiopathic pulmonary fibrosis (IPF) is a diagnosis and type of lung disease that occurs when doctors are unable to determine what is causing the scarring or fibrosis in the lungs. Patients with IPF often suffer from shortness of breath and a chronic, dry cough (21). Unfortunately, idiopathic pulmonary fibrosis is a progressive disease that worsens over time.
Researchers believe that IPF occurs after there has been recent damage to the air sacs in the lungs called alveoli. When this damage occurs, the immune system is triggered and sends an inflammatory response to heal the injury. For unknown reasons, this normal healing response begins to create scar tissue, leading to breathing issues in IPF patients (21).
Idiopathic pulmonary fibrosis is more commonly diagnosed in patients who are 50-60 years of age or older (21). Despite not knowing what triggers IPF, doctors believe there are several factors that may increase a patient’s risk. These risk factors include (21):
- Exposure to tobacco smoke
- Exposure to metal, wood, or dust
- Existing gastroesophageal reflux (GERD)
- Genetic mutations in the telomerase genes, surfactant genes, or mucin genes
- Hermansky Pudlak syndrome
- Environmental factors like smoking, chronic aspiration, viral infections
- Aging
- Exposure to radiation and chemotherapy
Interstitial Pulmonary Fibrosis
Non-idiopathic interstitial pulmonary fibrosis (non-IPF) is a term used to describe a group of interstitial lung diseases (ILD) that cause inflammation and fibrosis of the lung interstitium (1). The interstitium space of the lungs is the tissue that lines the walls of the alveoli and the blood vessels that transport oxygen throughout the body (38).
When interstitial pulmonary fibrosis occurs, the lining of the lungs becomes inflamed and scarred. This causes difficulty in breathing because the oxygen cannot easily pass through the scar tissue to the blood vessels that supply the body with oxygen (38). The inflammation and scarring of the lung tissue leads to the lung feeling stiff which causes shortness of breath and a dry cough.
Non-IPF can also affect the windpipe (trachea) and other lung tissues including the bronchi, bronchioles, alveoli, and pleural membranes (1). There are over 200 known causes of non-IPF including (1):
- Occupational & environmental exposures
- Exposure to inorganic substances, such as asbestos, beryllium, carbon dust, silica, and chromium
- Exposure to organic substances such as thermophilic fungi, bird droppings, and certain types of bacteria
- Drug-induced lung toxicity
- Some common drugs include (15):
- Statins for cholesterol
- Certain antibiotics such as nitrofurantoin & ethambutol
- Antineoplastic (anticancer) agents
- Beta-blockers such as amiodarone or propranolol
- Chemotherapy drugs including methotrexate & cyclophosphamide
- Anti-inflammatory drugs such as rituximab & sulfasalazine
- Radiation therapy
- Some common drugs include (15):
- Connective tissue diseases
- Systemic lupus erythematosus (SLE)
- Systemic sclerosis
- Rheumatoid arthritis
- Polymyositis & dermatomyositis
- Mixed connective tissue disease
- Systemic illnesses
- Sarcoidosis
- Pulmonary Langerhans cell histiocytosis
- Lymphangiomyomatosis
- Churg-Strass syndrome
- Chronic aspiration
- Alveolar proteinosis
Note: Veriheal does not intend to give this as professional medical advice. Do not attempt to self-diagnose, or prescribe treatment based on the information provided on this page. Always consult a physician before deciding on the treatment of a medical condition.
1. Agarwal, A. K., & Huda, N. (2023). Interstitial Pulmonary Fibrosis. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK557765/
2. Ali, A. M., El-Tawil, O. S., Al-Mokaddem, A. K., & Abd El-Rahman, S. S. (2021). Promoted inhibition of TLR4/miR-155/ NFkB p65 signaling by cannabinoid receptor 2 agonist (AM1241), aborts inflammation and progress of hepatic fibrosis induced by thioacetamide. Chemico-Biological Interactions, 336, 109398. https://doi.org/10.1016/j.cbi.2021.109398
3. Association, A. L. (n.d.-a). Marijuana and Lung Health. Retrieved May 3, 2023, from https://www.lung.org/quit-smoking/smoking-facts/health-effects/marijuana-and-lung-health
4. Association, A. L. (n.d.-b). Types, Causes and Risk Factors of Pulmonary Fibrosis. Retrieved April 17, 2023, from https://www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-fibrosis/introduction/types-causes-and-risk-factors
5. Barratt, S. L., Creamer, A., Hayton, C., & Chaudhuri, N. (2018). Idiopathic Pulmonary Fibrosis (IPF): An Overview. Journal of Clinical Medicine, 7(8), 201. https://doi.org/10.3390/jcm7080201
6. Cottin, V., Wollin, L., Fischer, A., Quaresma, M., Stowasser, S., & Harari, S. (2019). Fibrosing interstitial lung diseases: Knowns and unknowns. European Respiratory Review, 28(151). https://doi.org/10.1183/16000617.0100-2018
7. Could Cannabis Help People With Lung Diseases? | Pulmonary Fibrosis News. (n.d.). Retrieved April 17, 2023, from https://pulmonaryfibrosisnews.com/pulmonary-fibrosis-social-clips/cannabis-help-people-lung-diseases/
8. Fu, Q., Zheng, Y., Dong, X., Wang, L., & Jiang, C. G. (2017). Activation of cannabinoid receptor type 2 by JWH133 alleviates bleomycin-induced pulmonary fibrosis in mice. Oncotarget, 8(61), 103486–103498. https://doi.org/10.18632/oncotarget.21975
9. Garcia-Gonzalez, E., Selvi, E., Balistreri, E., Lorenzini, S., Maggio, R., Natale, M.-R., Capecchi, P.-L., Lazzerini, P.-E., Bardelli, M., Laghi-Pasini, F., & Galeazzi, M. (2009). Cannabinoids inhibit fibrogenesis in diffuse systemic sclerosis fibroblasts. Rheumatology (Oxford, England), 48(9), 1050–1056. https://doi.org/10.1093/rheumatology/kep189
10. Idiopathic Pulmonary Fibrosis | Pulmonary Fibrosis Foundation. (n.d.). Default. Retrieved April 17, 2023, from https://www.pulmonaryfibrosis.org/understanding-pff/types-of-pulmonary-fibrosis/idiopathic-pulmonary-fibrosis
11. Idiopathic Pulmonary Fibrosis – What Is Idiopathic Pulmonary Fibrosis? | NHLBI, NIH. (2022, March 24). https://www.nhlbi.nih.gov/health/idiopathic-pulmonary-fibrosis
12. Idiopathic pulmonary fibrosis, the endocannabinoid system and cannabinoids | Fundación CANNA: Scientific studies and cannabis testing. (n.d.). Retrieved April 17, 2023, from https://www.fundacion-canna.es/en/idiopathic-pulmonary-fibrosis-endocannabinoid-system-and-cannabinoids
13. Interstitial Lung Disease and Pulmonary Fibrosis | Columbia Surgery. (n.d.). Retrieved April 17, 2023, from https://columbiasurgery.org/conditions-and-treatments/interstitial-lung-disease-and-pulmonary-fibrosis
14. Interstitial Lung Disease: Pulmonary Fibrosis. (2021, August 8). https://www.hopkinsmedicine.org/health/conditions-and-diseases/interstitial-lung-disease-pulmonary-fibrosis
15. Interstitial lung disease—Symptoms and causes. (n.d.). Mayo Clinic. Retrieved April 17, 2023, from https://www.mayoclinic.org/diseases-conditions/interstitial-lung-disease/symptoms-causes/syc-20353108
16. Kalchiem-Dekel, O., Galvin, J. R., Burke, A. P., Atamas, S. P., & Todd, N. W. (2018). Interstitial Lung Disease and Pulmonary Fibrosis: A Practical Approach for General Medicine Physicians with Focus on the Medical History. Journal of Clinical Medicine, 7(12), 476. https://doi.org/10.3390/jcm7120476
17. Kaplan, A. G. (2021). Cannabis and Lung Health: Does the Bad Outweigh the Good? Pulmonary Therapy, 7(2), 395–408. https://doi.org/10.1007/s41030-021-00171-8
18. Kendall, R. T., & Feghali-Bostwick, C. A. (2014). Fibroblasts in fibrosis: Novel roles and mediators. Frontiers in Pharmacology, 5, 123. https://doi.org/10.3389/fphar.2014.00123
19. Kicman, A., Pędzińska-Betiuk, A., & Kozłowska, H. (2021). The potential of cannabinoids and inhibitors of endocannabinoid degradation in respiratory diseases. European Journal of Pharmacology, 911, 174560. https://doi.org/10.1016/j.ejphar.2021.174560
20. Kovalchuk, O., & Kovalchuk, I. (2020). Cannabinoids as anticancer therapeutic agents. Cell Cycle, 19(9), 961–989. https://doi.org/10.1080/15384101.2020.1742952
21. Krishna, R., Chapman, K., & Ullah, S. (2023). Idiopathic Pulmonary Fibrosis. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK448162/
22. Krzyżewska, A., Baranowska-Kuczko, M., Kasacka, I., & Kozłowska, H. (2022). Cannabidiol reduces lung and heart fibrosis in rats with monocrotaline-induced pulmonary hypertension. European Respiratory Journal, 60(suppl 66). https://doi.org/10.1183/13993003.congress-2022.4477
23. Li, X., Zhu, L., Wang, B., Yuan, M., & Zhu, R. (2017). Drugs and Targets in Fibrosis. Frontiers in Pharmacology, 8, 855. https://doi.org/10.3389/fphar.2017.00855
24. Luke, N. D., Vefali, B., Chow, P., Miller, R., Luke, N. D., Vefali, B., Chow, P., & Miller, R. (2023). Acute Recreational Cannabis-Induced Hypersensitivity Pneumonitis: A Case Report. Cureus, 15(4). https://doi.org/10.7759/cureus.37312
25. Mallat, A., Teixeira-Clerc, F., Deveaux, V., Manin, S., & Lotersztajn, S. (2011). The endocannabinoid system as a key mediator during liver diseases: New insights and therapeutic openings. British Journal of Pharmacology, 163(7), 1432–1440. https://doi.org/10.1111/j.1476-5381.2011.01397.x
26. Martinez-Pitre, P., Sabbula, B., & Cascella, M. (2022). Restrictive Lung Disease. StatPearls. https://www.statpearls.com/ArticleLibrary/viewarticle/90190
27. McGrail, J., Martín-Banderas, L., & Durán-Lobato, M. (2022). Cannabinoids as Emergent Therapy Against COVID-19. Cannabis and Cannabinoid Research, 7(5), 582–590. https://doi.org/10.1089/can.2022.0018
28. Montecucco, F., & Di Marzo, V. (2012). At the heart of the matter: The endocannabinoid system in cardiovascular function and dysfunction. Trends in Pharmacological Sciences, 33(6), 331–340. https://doi.org/10.1016/j.tips.2012.03.002
29. Nagarkatti, P., Pandey, R., Rieder, S. A., Hegde, V. L., & Nagarkatti, M. (2009). Cannabinoids as novel anti-inflammatory drugs. Future Medicinal Chemistry, 1(7), 1333–1349. https://doi.org/10.4155/fmc.09.93
30. Phan, T., Lau, K., & Li, X. (2005). Lung bullae and pulmonary fibrosis associated with marijuana smoking. Australasian Radiology, 49, 411–414. https://doi.org/10.1111/j.1440-1673.2005.01472.x
31. Pinheiro, G. A., Antao, V. C., Wood, J. M., & Wassell, J. T. (2008). Occupational Risks for Idiopathic Pulmonary Fibrosis Mortality in the United States. International Journal of Occupational and Environmental Health, 14(2), 117–123. https://doi.org/10.1179/oeh.2008.14.2.117
32. Preteroti, M., Wilson, E. T., Eidelman, D. H., & Baglole, C. J. (2023). Modulation of pulmonary immune function by inhaled cannabis products and consequences for lung disease. Respiratory Research, 24(1), 95. https://doi.org/10.1186/s12931-023-02399-1
33. Pryimak, N., Zaiachuk, M., Kovalchuk, O., & Kovalchuk, I. (2021). The Potential Use of Cannabis in Tissue Fibrosis. Frontiers in Cell and Developmental Biology, 9, 715380. https://doi.org/10.3389/fcell.2021.715380
34. Pulmonary Fibrosis. (n.d.). [Text]. National Library of Medicine. Retrieved April 17, 2023, from https://medlineplus.gov/pulmonaryfibrosis.html
35. Ribeiro, L. I., & Ind, P. W. (2016). Effect of cannabis smoking on lung function and respiratory symptoms: A structured literature review. Npj Primary Care Respiratory Medicine, 26(1), Article 1. https://doi.org/10.1038/npjpcrm.2016.71
36. Sido, J. M., Jackson, A. R., Nagarkatti, P. S., & Nagarkatti, M. (2016). Marijuana-derived Δ-9-tetrahydrocannabinol suppresses Th1/Th17 cell-mediated delayed-type hypersensitivity through microRNA regulation. Journal of Molecular Medicine (Berlin, Germany), 94(9), 1039–1051. https://doi.org/10.1007/s00109-016-1404-5
37. Turcotte, C., Blanchet, M.-R., Laviolette, M., & Flamand, N. (2016). The CB2 receptor and its role as a regulator of inflammation. Cellular and Molecular Life Sciences, 73(23), 4449–4470. https://doi.org/10.1007/s00018-016-2300-4
38. Understanding ILD. (n.d.). Interstitial Lung Disease Program. Retrieved April 17, 2023, from https://med.stanford.edu/ild/patient-resources/understanding-ild.html
39. Vuolo, F., Abreu, S., Michels, M., Xisto, D., Blanco, N., Hallak, J., Zuardi, A., Crippa, J., Reis, C., Bahl, M., Pizzichinni, E., Maurici, R., Pizzichinni, M., Rocco, P., & Dal-Pizzol, F. (2018). Cannabidiol reduces airway inflammation and fibrosis in experimental allergic asthma. European Journal of Pharmacology, 843. https://doi.org/10.1016/j.ejphar.2018.11.029
40. Wang, B., Kovalchuk, A., Li, D., Rodriguez-Juarez, R., Ilnytskyy, Y., Kovalchuk, I., & Kovalchuk, O. (2020). In search of preventive strategies: Novel high-CBD Cannabis sativa extracts modulate ACE2 expression in COVID-19 gateway tissues. Aging (Albany NY), 12(22), 22425–22444. https://doi.org/10.18632/aging.202225
41. Webb, M. B., Sickles, S., Weaver, C., & Osborn, J. (2020). Increased Pulmonary Function Following Administration of a CBD-Containing Compound NCMB-1 in Fibrotic Lungs of African Green Monkeys. The FASEB Journal, 34(S1), 1–1. https://doi.org/10.1096/fasebj.2020.34.s1.05699
42. Zurier, R. B., & Burstein, S. H. (2016). Cannabinoids, inflammation, and fibrosis. FASEB Journal: Official Publication of the Federation of American Societies for Experimental Biology, 30(11), 3682–3689. https://doi.org/10.1096/fj.201600646R