Marijuana (THC) After a Stroke: Does it Aid Recovery?
Cerebrovascular disease is a broad medical term used to describe various conditions that affect blood vessels inside the brain. Cerebral circulation is affected by cerebrovascular disease, as well as essential arteries that deliver oxygen and nutrients to the brain. The most common presentation of cerebrovascular disease is an ischemic stroke or transient ischemic attack (TIA).
According to the American Association of Neurological Surgeons (AANS), cerebrovascular disease is a leading cause of disability and the most common life-threatening neurological event in the United States. Stroke is the third leading cause of death across the nation. Approximately 500,000 of the 700,000 people affected yearly have never experienced a stroke before, whereas 200,000 experience recurrent attacks (3). Strikingly, 25% of first-time stroke patients will have another within 5 years.
Strokes affect African Americans and Hispanic Americans more often than any other ethnic group in the U.S. These ethnic groups, as well as people whose genetic bloodline extends across Asia, the Mediterranean, and the Middle East, are also more likely to develop sickle cell disease – a genetic condition that can interrupt blood flow due to narrowing of the arteries (10).
With the rise of medical marijuana legalization across the U.S. comes increased interest in using plant-based medicines for symptomatic relief from cardiovascular disease.
How Does the Endocannabinoid System (ECS) Play a Role in Treating Cerebrovascular Disease?
Everyone has a system in their body called the endocannabinoid system (ECS). This system consists of receptors that can be found in a variety of cells in the body. Cannabinoids, including medical cannabis, begin working by contacting specific receptors such as cannabinoid receptors CB1 & CB2, peroxisome proliferator-activated receptors (PPARs), and transient receptor potential (TRPs).
The receptors that are part of the ECS send signals that tell the body to increase or decrease the levels of naturally occurring, fatty-based neurotransmitters in the body called endocannabinoids. This process is responsible for regulating many processes in the body such as appetite, pain perception, and the immune system.
The ECS is part of a bigger system in the body called the endocannabinoidome (eCBome).
Medical cannabis contains over 120 different naturally occurring compounds called cannabinoids which include the famous Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD).
The ECS and eCBome may serve as a potential treatment option for patients with cerebrovascular disease. When a cerebrovascular event occurs, often brain tissues are damaged and begin to die. Through eCBome receptors and metabolic effects, researchers have found that THC and CBD may help limit the damage to nerve cells in the brain and potentially prevent stroke (36). This process is complex but it involves the activation of endocannabinoids and receptors that are able to decrease inflammation and stop brain cells from dying.
Additionally, research also suggests that medical cannabis activation of the ECS through the TRPV1 receptor causes the cells of the brain to release a vasodilator called calcitonin gene-related peptide (CGRP) (53). This is important as it can help decrease blood pressure in the brain after a blockage of blood flow.
Among all of the components contained in cannabis, CBD was found to be a good choice for patients suffering from cerebrovascular disease because of its ability to increase endocannabinoids and activate therapeutic eCBome receptors (36).
Are Cannabinoids a Good Treatment Option for Cerebrovascular Diseases Including Stroke?
Medical marijuana has the potential to become a strong treatment option for patients who have suffered from cerebrovascular diseases. Unfortunately, more research is needed to determine the safety and efficacy of humans. This is because many studies are conducted on animals and not all research is able to apply to humans at this time.
A 2016 review suggests that endocannabinoids play an important role in the regulation of blow flow in the brain (53). This is because all of the major types of cells that control cerebrovascular blood flow are capable of synthesizing endocannabinoids or have receptors that influence endocannabinoids.
Researchers believe that endocannabinoids have a strong potential to influence blood flow during a cerebrovascular event such as a stroke, traumatic brain injury, and vascular dementia (53).
It turns out that cannabinoids may also help with post-stroke pain and spasticity. In 2017, a group of researchers set out to see if nabiximols, a cannabis-based nasal spray, would be an effective add-on therapy for patients with uncontrollable muscle spasms and cramps (26).
Nabiximols, also known as Sativex, is available in 29 foreign countries including in the EU and Canada as a prescription for spasticity associated with multiple sclerosis (MS) (20). It is an effective cannabis-based medication but is only officially approved for very few medical conditions.
The double-blind, placebo-controlled, crossover study included a total of 37 patients who were experiencing spasticity that was caused by a stroke (26). Patients were assessed for stretch reflex spasticity, range of motion, pain, sleep and bladder function, and the frequency of spasticity attacks.
Each patient received 4 weeks of a 1:1 THC: CBD oro-mucosal nabiximols and a placebo nasal spray, with a 2-week washout period in between (26). Completed study results published in 2022 found that nabiximols is safe, but it is not effective for use in stroke patients. Researchers believe that nabiximols could have provided stronger results if more patients with more severe spasticity levels were included in the study (27).
A case study examining nabiximols use was published in 2021. This study tested nabiximols in a 61-year-old experiencing central post-stroke pain syndrome (28). This patient experienced a burning and shooting pain in their leg and face and had taken amitriptyline, gabapentin, pregabalin, and various opioids for over 3 years.
After 2 days of nabiximols treatment, the patient reported a marked improvement in pain intensity, mood, daily activity, quality of life, and sleep (28). The patient did not need any additional medications to achieve the levels of relief they experienced and were monitored for 10 months.
These studies on nabiximols are very promising for those who are thinking about using medical cannabis in relation to the pain and spasticity they experience after having a stroke.
Does Medical Cannabis Increase the Risk of Stroke?
There are mixed opinions on whether cannabis use increases the risk of cerebrovascular events, such as acute stroke, in younger patients. Using cannabis has been associated with ischemic and hemorrhagic stroke in younger individuals (29). Cannabis use has also been associated with increased risk for patients with cardiovascular disease. It is important to disclose any cannabis use with your doctor for these reasons.
A 2021 study found that marijuana use was not associated with early-onset ischemic stroke using limited population data (9).
A different study published in 2020 studied whether there is an association between recent cannabis use and acute ischemic stroke (25). This study retrospectively examined 9,350 stroke patients and cannabis use presence through urine drug screen. Unadjusted results (not factoring in age or other medical demographics) found a 50% decrease in stroke risk among cannabis users. Only 18% or 1,643 acute ischemic stroke patients were cannabis users, only determined by urine drug screen.
What Cannabis Preparations Are Suitable for Cerebrovascular Disease & Stroke?
One of the main appeals associated with medical cannabis use to treat the symptoms of cerebrovascular disease is the diversity in terms of product options. Various cannabis preparations are available:
- Edibles
- Pills, capsules, and tablets
- Powder Cannabis powder
- Transdermal Patches
- Vapes
- Tinctures
Talking to Your Doctor About Diagnosing Cerebrovascular Disease
One or numerous cerebral blood vessels must be involved in the pathological process for a doctor to diagnose conditions of this kind. Most cerebrovascular problems can be confirmed after you’ve undergone some diagnostic imaging tests and answered personal family health questionnaires.
Neurologists and surgeons can conduct the following tests to view the arteries and vessels in and around the brain, as well as those found on the actual brain tissue:
- Cerebral angiography
- Carotid duplex (also called carotid ultrasound)
- Computed tomography angiogram (CT or CAT scan)
- Doppler ultrasound
- Magnetic Resonance Imaging (MRI)
- Magnetic Resonance Angiogram (MRA)
Complementary Treatments Worth Discussing with Your Doctor
Stroke survivors often search for complementary and alternative interventions (CAIs), particularly if they are unsatisfied with their treatment regimen or the progress of their healing journey. Cannabinoids with neuroprotective qualities could be considered as a form of complementary therapy but should not be used as a replacement for existing medications nor emergency stroke care.
The Institute for Integrative Healthcare Studies supports the idea of integrating reflexology, aromatherapy, and Shiatsu into post-stroke recovery plans (41). Complementary and alternative therapies for poststroke depression include cannabis rich in CBD, which has been shown to exert anxiolytic and neuroprotective, anti-inflammatory effects in users.
A meta-analysis of traditional Chinese medicines for ischaemic stroke displayed noticeable improvement in neurological deficits on stroke scales (48). There was, however, no evidence spotlighting the benefits of Ayurveda, homeopathy, or reiki for people with cerebrovascular disease.
Keep in mind that while medical marijuana and other complementary medicines can prove beneficial for you or a loved one with cerebrovascular disease, including stroke, it’s important that you continue using any medications or treatments that are prescribed by your doctor.
What is Cerebrovascular Disease?
The term cerebrovascular disease encompasses several different conditions that can cause damage to the blood vessels and arteries of the brain. It is possible for patients of any age and gender to experience these problems. Some forms of cerebrovascular disease are present at birth, while others can occur without warning later in life.
Stroke is considered the most common cause of cerebrovascular disease. Other types include (4):
- Transient ischemic attack (TIA)
- Colloquially but inaccurately also known as a mini-stroke
- Brain aneurysm
- Arteriovenous malformation (AVM)
- Brain bleeds or hemorrhages
- Intracranial hemorrhage
- Subarachnoid hemorrhage (SAH)
- Reversible cerebral vasoconstriction syndrome (RCVS)
- Carotid artery disease
- Cervical artery dissection
- Hereditary hemorrhagic telangiectasia
- Moyamoya disease
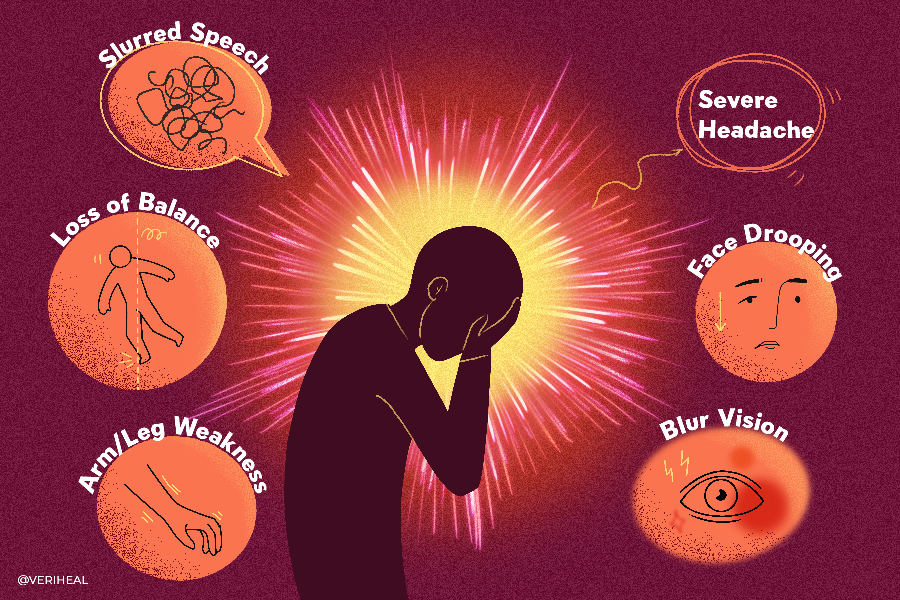
The symptoms of cerebrovascular disease tend to vary based on what area of the brain is affected (4). Some of the symptoms patients may experience include (4):
- Problems with balance
- Vision problems including vision loss, or double vision
- Sudden and severe headache
- Aphasia – trouble speaking or understanding speech
- Slurred speech
- Paralysis or weakness on one side of the body or face
- Sensory changes on one side of the body or face
If you experience any of these symptoms, it is important to visit the emergency department right away. Cerebrovascular disease is a medical emergency and needs to be addressed promptly to avoid permanent damage or death.
Stroke
A stroke happens when blood flow is restricted to a certain part of your brain (ischemia). When the blood is lacking oxygen, brain cells quickly start dying (3).
Restrictions in blood flow may occur from blockage (embolism), blood vessel rupture (hemorrhage), clot formation (thrombosis), and vessel narrowing (stenosis).
Strokes are characterized by sudden onset of symptoms. Your likelihood of survival and functional outcomes will be time-sensitive, proving the importance of getting a diagnosis as soon as you notice the symptoms. Some of the symptoms of a stroke or transient ischemic attack (TIA) include (42, 43):
- Confusion and memory loss
- Dizziness
- Difficulty walking or inability to walk
- Headache
- Speech impairment
- Tingling and numbness in the arm, face, or leg (typically on one side of the body)
- Vision problems
- Vomiting and nausea
Spotting A Stroke
To help you spot the warning signs of a stroke, it’s worth learning the meaning of the acronym “FAST” (42):
- Facial sag – One side of the face may appear “saggy”, making it difficult for the affected person to smile.
- Arm weakness – Patients who suffer a stroke will be unable to raise their arm above their head
- Speech difficulty – Stroke can have a major impact on speech, with many patients unable to pronounce words correctly.
- Time to call 911 – Don’t hesitate to seek medical attention if you notice one or more of these symptoms.
Stroke Causes
A stroke can occur at any time, but there are certain lifestyle choices and medical conditions that may increase your risk. The risk factors for stroke include (4):
- High blood pressure
- High cholesterol
- Tobacco smoking or chewing
- Heart disease
- Diabetes
- Obesity
- Taking blood-thinning medications such as warfarin and certain non-steroidal anti-inflammatory (NSAIDs) such as ibuprofen
- Hormone therapy
- Age
- Genetics
- Gender
- Race
Note: Veriheal does not intend to give this as professional medical advice. Do not attempt to self-diagnose or prescribe treatment based on the information provided on this page. Always consult a physician before making any decision on the treatment of a medical condition.
1. Blood Pressure Medications: A List. (n.d.). Retrieved August 15, 2023, from https://www.healthline.com/health/high-blood-pressure-hypertension-medication
2. Capettini, L. S. A., Savergnini, S. Q., da Silva, R. F., Stergiopulos, N., Santos, R. A. S., Mach, F., & Montecucco, F. (2012). Update on the Role of Cannabinoid Receptors after Ischemic Stroke. Mediators of Inflammation, 2012, e824093. https://doi.org/10.1155/2012/824093
3. Cerebrovascular Disease – Classifications, Symptoms, Diagnosis and Treatments. (n.d.). Retrieved October 30, 2023, from https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Cerebrovascular-Disease
4. Cerebrovascular Disease: Types, Causes & Symptoms. (n.d.). Cleveland Clinic. Retrieved August 15, 2023, from https://my.clevelandclinic.org/health/diseases/24205-cerebrovascular-disease
5. Chiu, R. G., Fuentes, A. M., Patil, S. N., Chiu, R., McGuire, L. S., & Mehta, A. I. (2022). Cannabis Abuse and Perioperative Complications After Treatment of Intracranial Aneurysms: A Nationwide Analysis. World Neurosurgery, 158, e184–e195. https://doi.org/10.1016/j.wneu.2021.10.156
6. Choi, S.-H., Mou, Y., & Silva, A. C. (2019). Cannabis and Cannabinoid Biology in Stroke. Stroke, 50(9), 2640–2645. https://doi.org/10.1161/STROKEAHA.118.023587
7. Contributors, W. E. (n.d.). Stroke: Know What Puts You at Most Risk. WebMD. Retrieved August 15, 2023, from https://www.webmd.com/stroke/stroke-causes-risks
8. De Luca, M. A., & Fattore, L. (2018). Therapeutic Use of Synthetic Cannabinoids: Still an Open Issue? Clinical Therapeutics, 40(9), 1457–1466. https://doi.org/10.1016/j.clinthera.2018.08.002
9. Dutta, T., Ryan, K. A., Thompson, O., Lopez, H., Fecteau, N., Sparks, M. J., Chaturvedi, S., Cronin, C., Mehndiratta, P., Nunez Gonzalez, J. R., Phipps, M., Wozniak, M., McArdle, P. F., Kittner, S. J., & Cole, J. W. (2021). Marijuana Use and the Risk of Early Ischemic Stroke. Stroke, 52(10), 3184–3190. https://doi.org/10.1161/STROKEAHA.120.032811
10. Effects of Stroke. (2022, December 22). https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/effects-of-stroke
11. England, T. J., Hind, W. H., Rasid, N. A., & O’Sullivan, S. E. (2015). Cannabinoids in Experimental Stroke: A Systematic Review and Meta-Analysis. Journal of Cerebral Blood Flow & Metabolism, 35(3), 348–358. https://doi.org/10.1038/jcbfm.2014.218
12. Faroqui, R., Mena, P., Wolfe, A. R., Bibawy, J., Visvikis, G. A., & Mantello, M. T. (2018). Acute carotid thrombosis and ischemic stroke following overdose of the synthetic cannabinoid K2 in a previously healthy young adult male. Radiology Case Reports, 13(3), 747–752. https://doi.org/10.1016/j.radcr.2018.02.023
13. Feng Wang, Jing Han, Haruki Higashimori, Jingyi Wang, Jingjing Liu, Li Tong, Yongjie Yang, Hailong Dong, Xia Zhang, Lize Xiong. Long-term depression induced by endogenous cannabinoids produces neuroprotection via astroglial CB1R after stroke in rodents (2019). Retrieved August 15, 2023, from https://journals.sagepub.com/doi/full/10.1177/0271678X18755661
14. Fernández-Ruiz, J., Moro, M. A., & Martínez-Orgado, J. (2015). Cannabinoids in Neurodegenerative Disorders and Stroke/Brain Trauma: From Preclinical Models to Clinical Applications. Neurotherapeutics, 12(4), 793–806. https://doi.org/10.1007/s13311-015-0381-7
15. Frontiers | Harmful Effects of Smoking Cannabis: A Cerebrovascular and Neurological Perspective. (n.d.). Retrieved August 15, 2023, from https://www.frontiersin.org/articles/10.3389/fphar.2019.01481/full
16. Good, D. C. (1990). Cerebrovascular Disease. In H. K. Walker, W. D. Hall, & J. W. Hurst (Eds.), Clinical Methods: The History, Physical, and Laboratory Examinations (3rd ed.). Butterworths. http://www.ncbi.nlm.nih.gov/books/NBK378/
17. Guerram, M., Zhang, L.-Y., & Jiang, Z.-Z. (2016). G-protein coupled receptors as therapeutic targets for neurodegenerative and cerebrovascular diseases. Neurochemistry International, 101, 1–14. https://doi.org/10.1016/j.neuint.2016.09.005
18. Hillard, C. J. (2008). Role of cannabinoids and endocannabinoids in cerebral ischemia. Current Pharmaceutical Design, 14(23), 2347–2361. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2581413/
19. Járai, Z., Wagner, J. A., Varga, K., Lake, K. D., Compton, D. R., Martin, B. R., Zimmer, A. M., Bonner, T. I., Buckley, N. E., Mezey, E., Razdan, R. K., Zimmer, A., & Kunos, G. (1999). Cannabinoid-induced mesenteric vasodilation through an endothelial site distinct from CB1 or CB2 receptors. Proceedings of the National Academy of Sciences of the United States of America, 96(24), 14136–14141. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC24203/
20. Jazz Pharmaceuticals Announces Top-line Results from Phase 3 Trial Evaluating Nabiximols Oromucosal Spray in Adult Participants with Multiple Sclerosis Spasticity | Jazz Pharmaceuticals plc. (n.d.). Retrieved October 30, 2023, from https://investor.jazzpharma.com/news-releases/news-release-details/jazz-pharmaceuticals-announces-top-line-results-phase-3-trial/
21. JCM | Free Full-Text | A Mechanistic and Pathophysiological Approach for Stroke Associated with Drugs of Abuse. (n.d.). Retrieved August 15, 2023, from https://www.mdpi.com/2077-0383/8/9/1295
22. Khaku, A. S., & Tadi, P. (2023). Cerebrovascular Disease. In StatPearls. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK430927/
23. Latorre, J. G. S., & Schmidt, E. B. (2015). Cannabis, Cannabinoids, and Cerebral Metabolism: Potential Applications in Stroke and Disorders of the Central Nervous System. Current Cardiology Reports, 17(9), 72. https://doi.org/10.1007/s11886-015-0627-3
24. Feng Wang, Jing Han, Haruki Higashimori, Jingyi Wang, Jingjing Liu, Li Tong, Yongjie Yang, Hailong Dong, Xia Zhang, Lize Xiong. Long-term depression induced by endogenous cannabinoids produces neuroprotection via astroglial CB1R after stroke in rodents (2019). Retrieved August 15, 2023, from https://journals.sagepub.com/doi/full/10.1177/0271678X18755661
25. Luis, C. V. S., Nobleza, C. O. S., Shekhar, S., Sugg, R., Villareal, D. J., Mehta, T., & Gangadhara, S. (2020). Association between recent cannabinoid use and acute ischemic stroke. Neurology: Clinical Practice, 10(4), 333–339. https://doi.org/10.1212/CPJ.0000000000000888
26. Marinelli, L., Balestrino, M., Mori, L., Puce, L., Rosa, G. M., Giorello, L., Currà, A., Fattapposta, F., Serrati, C., Gandolfo, C., Abbruzzese, G., & Trompetto, C. (2017). A randomised controlled cross-over double-blind pilot study protocol on THC:CBD oromucosal spray efficacy as an add-on therapy for post-stroke spasticity. BMJ Open, 7(9), e016843. https://doi.org/10.1136/bmjopen-2017-016843
27. Marinelli, L., Puce, L., Mori, L., Leandri, M., Rosa, G. M., Currà, A., Fattapposta, F., & Trompetto, C. (2022). Cannabinoid Effect and Safety in Spasticity Following Stroke: A Double-Blind Randomized Placebo-Controlled Study. Frontiers in Neurology, 13. https://www.frontiersin.org/articles/10.3389/fneur.2022.892165
28. Moser, U. (2021). Tetrahydrocannabinol and cannabidiol as an oromucosal spray in a 1:1 ratio: A therapeutic option for patients with central post-stroke pain syndrome? BMJ Case Reports, 14(7), e243072. https://doi.org/10.1136/bcr-2021-243072
29. Moustafa, B., & Testai, F. D. (2021). Cerebrovascular Complications Associated with Marijuana Use. Current Neurology and Neuroscience Reports, 21(6), 25. https://doi.org/10.1007/s11910-021-01113-2
30. Pérez-Neri, I., Estêvão, M. D., Mishra, R., Sandoval, H., Zárate, M., & Ríos, C. (2023). Therapeutic potential of cannabinoids for stroke: Scoping review protocol. Archivos de Neurociencias, 28(2), Article 2. https://doi.org/10.31157/an.v28i2.356
31. Pharmaceutics | Free Full-Text | Cannabinoids, Blood–Brain Barrier, and Brain Disposition. (n.d.). Retrieved August 15, 2023, from https://www.mdpi.com/1999-4923/12/3/265
32. Pini, A., Mannaioni, G., Pellegrini-Giampietro, D., Beatrice Passani, M., Mastroianni, R., Bani, D., & Masini, E. (2012). The Role of Cannabinoids in Inflammatory Modulation of Allergic Respiratory Disorders, Inflammatory Pain and Ischemic Stroke. Current Drug Targets, 13(7), 984–993. https://doi.org/10.2174/138945012800675786
33. Pires, P. W. (2018). Cannabinoids during ischemic strokes: Friends or foes? American Journal of Physiology-Heart and Circulatory Physiology, 314(6), H1155–H1156. https://doi.org/10.1152/ajpheart.00107.2018
34. Ronca, R. D., Myers, A. M., Ganea, D., Tuma, R. F., Walker, E. A., & Ward, S. J. (2015). A selective cannabinoid CB2 agonist attenuates damage and improves memory retention following stroke in mice. Life Sciences, 138, 72–77. https://doi.org/10.1016/j.lfs.2015.05.005
35. Sang-Ho, Choi, Yongshan, Mou, & Silva, Alfonso. Cannabis and Cannabinoid Biology in Stroke | Stroke. (2019). Retrieved August 15, 2023, from https://www.ahajournals.org/doi/10.1161/STROKEAHA.118.023587
36. Scharf, E. L. (2017). Translating Endocannabinoid Biology into Clinical Practice: Cannabidiol for Stroke Prevention. Cannabis and Cannabinoid Research, 2(1), 259–264. https://doi.org/10.1089/can.2017.0033
37. Shuai Yang, Zongming Wang, Changming Zhang, Haosen Jiao, Liguang Wei, Ji Jia, & Jingling Zhao. Cannabinoid CB1 receptor agonist ACEA alleviates brain ischemia/reperfusion injury via CB1–Drp1 pathway | Cell Death Discovery. (2020). Retrieved August 15, 2023, from https://www.nature.com/articles/s41420-020-00338-3
38. Slayden, A., Mysiewicz, S., North, K., Dopico, A., & Bukiya, A. (2022). Cerebrovascular Effects of Alcohol Combined with Tetrahydrocannabinol. Cannabis and Cannabinoid Research. https://doi.org/10.1089/can.2021.0234
39. Stanley, C. P., Hind, W. H., Tufarelli, C., & O’Sullivan, S. E. (2015). Cannabidiol causes endothelium-dependent vasorelaxation of human mesenteric arteries via CB1 activation. Cardiovascular Research, 107(4), 568–578. https://doi.org/10.1093/cvr/cvv179
40. Stroke Health Center—WebMD. (n.d.). Retrieved August 15, 2023, from https://www.webmd.com/stroke/default.htm
41. Stroke Rehabilitation: 3 Complementary Therapies. (2008, May 21). Massage Professionals Update. https://www.integrativehealthcare.org/mt/massage-essential-oils-stroke-patient/
42. Stroke Symptoms and Warning Signs. (n.d.). Www.Stroke.Org. Retrieved August 17, 2023, from https://www.stroke.org/en/about-stroke/stroke-symptoms
43. Stroke: What It Is, Causes, Symptoms, Treatment & Types. (n.d.). Retrieved August 17, 2023, from https://my.clevelandclinic.org/health/diseases/5601-stroke
44. Sultan, S. R., Millar, S. A., England, T. J., & O’Sullivan, S. E. (2017). A Systematic Review and Meta-Analysis of the Haemodynamic Effects of Cannabidiol. Frontiers in Pharmacology, 8. https://doi.org/10.3389/fphar.2017.00081
45. Swetlik, C., Migdady, I., Hasan, L. Z., Buletko, A. B., Price, C., & Cho, S.-M. (2022). Cannabis Use and Stroke: Does a Risk Exist? Journal of Addiction Medicine, 16(2), 208–215. https://doi.org/10.1097/ADM.0000000000000870
46. The Cannabinoid WIN55212-2 Promotes Neural Repair After Neonatal Hypoxia–Ischemia | Stroke. (n.d.). Retrieved August 15, 2023, from https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.110.599357
47. Top 10 Causes of Strokes—Risk Factors and How You Can Lower Your Risks. (n.d.). Retrieved August 15, 2023, from https://www.webmd.com/stroke/stroke-causes-risks
48. Venketasubramanian, N. (2021). Complementary and alternative interventions for stroke recovery—A narrative overview of the published evidence. Journal of Complementary & Integrative Medicine, 18(3), 553–559. https://doi.org/10.1515/jcim-2020-0062
49. Vicente-Acosta, A., Ceprian, M., Sobrino, P., Pazos, M. R., & Loría, F. (2022). Cannabinoids as Glial Cell Modulators in Ischemic Stroke: Implications for Neuroprotection. Frontiers in Pharmacology, 13. https://www.frontiersin.org/articles/10.3389/fphar.2022.888222
50. Ward, S. J., Castelli, F., Reichenbach, Z. W., & Tuma, R. F. (2018). Surprising outcomes in cannabinoid CB1/CB2 receptor double knockout mice in two models of ischemia. Life Sciences, 195, 1–5. https://doi.org/10.1016/j.lfs.2017.12.030
51. Zarruk, J. G., Fernández-López, D., García-Yébenes, I., García-Gutiérrez, M. S., Vivancos, J., Nombela, F., Torres, M., Burguete, M. C., Manzanares, J., Lizasoain, I., & Moro, M. A. (2012). Cannabinoid Type 2 Receptor Activation Downregulates Stroke-Induced Classic and Alternative Brain Macrophage/Microglial Activation Concomitant to Neuroprotection. Stroke, 43(1), 211–219. https://doi.org/10.1161/STROKEAHA.111.631044
52. Zhang, M., Martin, B. R., Adler, M. W., Razdan, R. J., Kong, W., Ganea, D., & Tuma, R. F. (2009). Modulation of Cannabinoid Receptor Activation as a Neuroprotective Strategy for EAE and Stroke. Journal of Neuroimmune Pharmacology, 4(2), 249–259. https://doi.org/10.1007/s11481-009-9148-4
53. Zoltán Benyó, Éva Ruisanchez, Miriam Leszl-Ishiguro, Péter Sándor, and Pál Pacher. Endocannabinoids in cerebrovascular regulation | American Journal of Physiology-Heart and Circulatory Physiology. (2016). Retrieved August 15, 2023, from https://journals.physiology.org/doi/full/10.1152/ajpheart.00571.2015